From its beginnings sixty years ago, Barton Health’s commitment to the community has never wavered.
At times, the residents of Lake Tahoe literally put hammer to nail to create the first-ever health care facility in these splendid mountains. In doing so, they ensured a better future for themselves, their families, and future generations.
In 1960, when the Barton-Ledbetter family donated a tract of farmland to build a community hospital, they set the stage for everything that followed: 60 years of progress and pride, growth and change, occasional setbacks, and incredible advances.
As we celebrate this pivotal milestone—the first 60 years of health care service to the region—please join us in looking back at our rich history and looking ahead to a bright future.
IN THE BEGINNING
From Homestead to Home of Healthcare
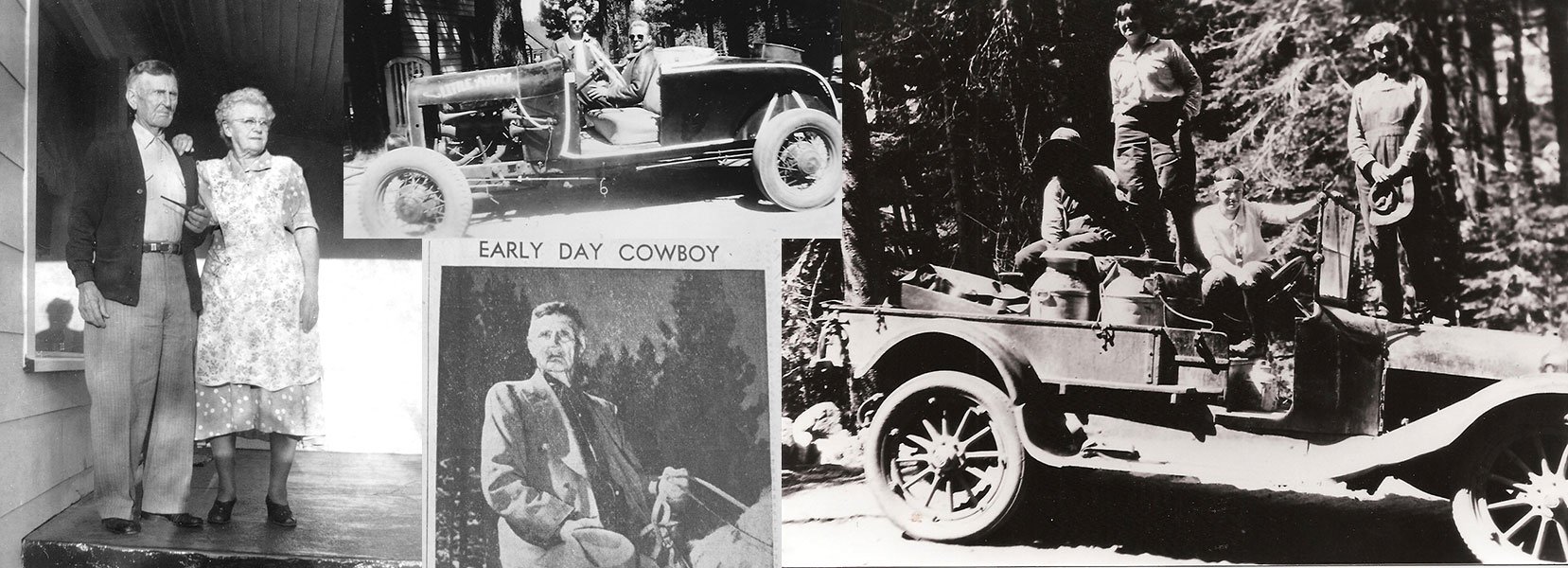
When William D. Barton and Ouida Leona Kyburz got married in 1902, they could not have imagined the legacy their partnership would create for generations to come. In 1960, their daughters, Fay and Alva, made that legacy a reality with a generous land donation. The six-acre tract, given in memory of their late parents, would soon be home to Lake Tahoe’s first hospital.
Last of the Pioneers
The Barton story began—and could have ended— two generations earlier, when Ouida’s parents headed West with the wagon train pioneers. When they reached the Sierra Nevada, the Kyburz family parted company with the ill-fated Donner party, with whom they had traveled across the country. Had they chosen differently, it could have meant a different outcome for the Kyburz family. However, they successfully made it over the mountains, Ouida was born, and many years later she met and married William Barton, engraving their place in Barton Health’s history.
Bill was one of the last of the Lake Tahoe range pioneers. As a young boy, he worked the family cattle drives. As an adult, he relocated from Folsom to Lake Tahoe to spend his summers in the high mountain pastures. The rugged cowboy eventually settled and built his 1,000-acre Lyon’s Ranch near the Southwest side of Lake Tahoe’s South Shore. Each year, when fall settled in, he and his family—including daughters Fay and Alva—would return to Folsom for the winter.
In addition to their daughters, Bill and Ouida Barton adopted a 9-year-old boy, Jesse Riola. A gentle youngster with a zest for life, Jesse joined the ranch hands when he got older; Fay and Alva were also ranchers and experienced horsewomen who delivered dairy products throughout South Lake Tahoe for the family-owned Lake Valley Creamery.
As the daughters once recounted, they fully understood how vulnerable they were living in the high mountain terrain when their father fell from a horse and broke his leg. Bill, then 81, was transported in an ambulance more than 140 miles to Sacramento. After surgery, he refused to return to Tahoe by ambulance. Instead, he made the arduous journey in the back of a pickup truck driven by daughter Fay, with a large umbrella for protection from the sun—a sight that drew stares from curious onlookers.
Other medical emergencies—their mother, Ouida, once fell from a horse and broke her back, and their grandmother broke her neck tumbling down a flight of stairs—made the sisters keenly aware of the need for accessible local health care.
Building a Legacy
When residents of Lake Tahoe first began talking about building a hospital in the region, Fay Ledbetter and Alva Barton knew there was an opportunity to provide an essential asset to their community. In 1961, they graciously stepped forward with the offer of a six-acre land parcel for the hospital construction. The gift, valued at nearly $200,000, would be a catalyst for the hospital fund-raising effort.
As the campaign moved forward, what was originally conceived as Lake Tahoe Community Hospital would be renamed Barton Memorial Hospital. Not only would Fay and Alva make history with their contribution, Fay’s son, William B. Ledbetter, would help lead ongoing efforts for fund-raising and additional construction over the next five decades.
The Barton-Ledbetter family has remained active with the hospital throughout its first 50 years. Ledbetter remained on the hospital board of directors from 1960 to 1989. When the Barton Memorial Hospital Foundation was incorporated in 1990, he served as the founding chairman. He continued to serve as the general manager for Harvey’s, a local hotel and casino, until he retired in 2007. Art and landscaping were Ledbetter’s passions, and he chaired the Barton Foundation Art Committee, which placed original works of donated and purchased art throughout the hospital.
A Family Tradition
The Barton family’s support of its namesake medical facility started over six decades ago and continues today through generations of Bartons and Ledbetters.
Benefactors Alva Barton and Fay Barton Ledbetter lived long and fruitful lives after donating the original tract of land where Barton Memorial Hospital was built. Alva pursued a teaching career and lived in Sacramento. She frequented South Shore in the summers, living in the family’s historic home. She traveled often with her sister, loved spending time with family, and maintained a good sense of humor until she died at age 97.
Fay married and settled in Sloughhouse, California. She continued to work on the family dairy farm until age 75 and remained actively involved in the family business until age 90.
Jesse Riola Barton, Bill and Ouida’s adopted son, was the one person who remained by Bill’s side through his final days. His niece, Melba Ledbetter Mosher, referred to “Uncle Jesse” in the most loving terms.
Bill Ledbetter, Fay’s son, married Beverlee Gross in 1954. They had two daughters, Jessica and Erica, and a son, Kirk. Bill worked tirelessly to garner support for a hospital in Tahoe.
In 1998, the Beverlee Ledbetter Memorial Playground was built on the hospital site. The playground was constructed by volunteers with funds donated by the family, as well as memorial gifts given in Beverlee's name.
Jessica followed in her father’s footsteps by serving on the hospital board of directors for 15 years, from 1989 to 2004. Kirk joined the board in 2008 and continues to serve in that capacity today.
In 2008, in memory of their parents, Bill and Beverlee, and their sister, Erica Faye Ledbetter, who passed before her time, Jessica and Kirk Ledbetter funded the healing gardens at the entrance of the Barton Skilled Nursing Facility. With its elegant park-like atmosphere, complete with a cascading waterfall, the healing gardens provide a warm, comforting welcome to patients, visitors, and residents.
1950s-1963 - MIRACLE IN THE MOUNTAINS
A drive through the Sierra Nevada always assures spectacular views. But a journey through those same mountains to reach a hospital more than an hour away could be filled with tension. That was Lake Tahoe before Barton Memorial Hospital.
During the 1950s, Tahoe’s full-time population was estimated at just 100 households, though the influx of summer visitors could easily reach 5,000. Then the region began to grow. Tourism, professional services, the construction industry, and thriving casinos enticed newcomers and entrepreneurs. As more people settled in Tahoe, a community hospital became vital.
In 1958, Lawrence Janus, M.D., became the first physician to commit to year-round residency in Lake Tahoe. For a time, Dr. Janus was the sole physician through the long, cold winter and busy summer. Dr. Janus has shared stories of chasing 7-year-old Randy Butler through the woods to give him a flu shot; Randy ran out of the doctor’s office after seeing the needle.
At that time, patient payments were frequently based on the barter system. In 1957, when residents picked up their hammers to construct Tahoe Medical Clinic, funds came from a side of beef donated by Bill Barton and prepared by butcher Harvey Gross. And one night Dr. Janus returned home with a sewing machine for his wife in lieu of payment.
In late 1959, James Whitely, M.D., moved permanently to South Lake Tahoe. Whenever an accident occurred, the doctor used his own car, loaded with emergency equipment, sometimes escorted by the fire department or police. When people were injured at Desolation Wilderness, Dr. Whitely was flown in by helicopter. And when the outcome was unfortunate, Dr. Whitely and his wife Patricia even opened their home for grief support for those awaiting the Placerville coroner.
In those days, practicing medicine in Tahoe was no easy task. Doctors did not get much rest, and often had no backup physicians to assist. Peter Irving, M.D., for example, who would later serve as the hospital’s first general surgeon, performed all his surgeries at Carson Hospital, located in Eagle Valley, until Barton opened. He shared the story of a young boy who needed an emergency appendectomy. Dr. Irving loaded the child into his Volkswagen Beetle and rushed to Carson City to perform surgery.
In the early days of Tahoe health care, doctors did what had to be done under dire circumstances. Acting as personal taxi drivers to distant hospitals was just part of the job. Though the pioneer days had passed, this was still frontier medicine.
Building the Case for a Hospital
Within a few years, five medical doctors and three doctors of osteopathy had joined the Tahoe clinic staff. They delivered urgent health care, treated emergencies, and though the clinic was not designed for surgery, also performed tonsillectomies and last-minute deliveries. The clinic became the destination of choice for patients when emergencies prevented the long trip over two-lane Spooner Summit, the only pass linking Lake Tahoe to the greater Carson area.
Meanwhile, Dr. Whitely was building a case for a local hospital, and the community rallied in support. They realized that in serious and critical cases, the hospitals in Carson City and Placerville—each an hour or more from Lake Tahoe—were simply too far away.
According to patient records from 1959, 1,500 emergency visits to Carson Hospital were from South Lake Tahoe—nearly one-third of the hospital’s emergency room usage. From May 1959 to May 1960, Carson Hospital’s patient admissions from the South Shore totaled 467. Many lives were lost during transport to Placerville and Carson City. Emergencies, accidents, and even childbirth did not always have positive outcomes due to the long distance necessary to travel for services.
The need for a hospital was abundantly clear, but proponents still needed to sell the concept. Putting pen to paper, they presented their case: A hospital would provide 24-hour medical care; emergency care would be easily accessible; broken bones, infections, burns, and illnesses would be treated locally; blood infusions, anesthesia, laboratory tests, and X-rays would all be available; and business owners would benefit from fewer lost workdays among staff due to travel for treatments, diagnostic tests, and follow-up care. Although the opinion was not unanimous, most locals felt a modern hospital would be a valuable resource for the community.
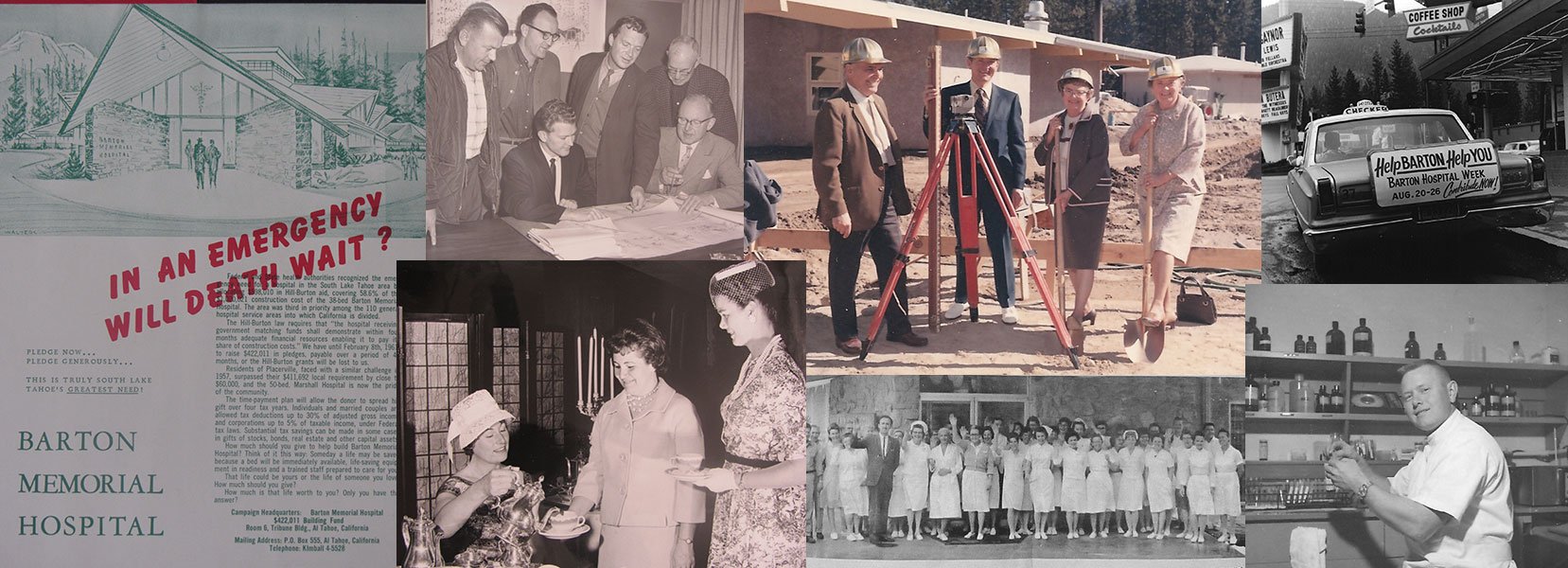
By October 1960 the community was organized, serious, and committed to building a hospital at Lake Tahoe. Prominent business leader Lee DeLauer was selected to head the Hospital Organizing Committee. He and his 16-member Volunteer Incorporating Committee partnered to make the venture a success.
Research conducted by Gene Morrison, a businessman with a passion for the health of local residents, found that almost $600,000 in building funds was available from the federal and state governments. The caveat: Local fund-raising would have to pay for at least one-third of the total. No one thought the task would be easy, and some thought it would be nearly impossible. But “impossible” was not in the vocabulary of most Lake Tahoe residents.
Estimates showed that the hospital would cost more than $1 million. While federal Hill-Burton funding and state grants amounted to $598,010 (58.6 percent of the cost), the community fund-raising campaign would have to reach $422,011 in donations (41.4 percent) by February 8, 1962, just four months later, or South Tahoe would not be eligible for the funding for another decade. That deadline motivated the team to raise the money immediately.
Then, sisters Fay Ledbetter and Alva Barton stepped up with a parcel of farmland in an easily accessible area—the perfect site for a future hospital. The property was assessed at nearly $200,000. The fund-raising had officially started.
Voice of the People
The proposed Lake Tahoe Community Hospital was the topic of conversation in coffee shops, on Main Street, and at family dinner tables.
By October 1960, a chief of staff was appointed to be responsible for oversight of doctors. The resolution created open and dual staff privileges for the hospital consisting of physicians, surgeons, and other competent doctors.
The composition of the medical staff also was key to accreditation by The Joint Commission, previously known as the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), which oversees standards of care, processes, and accountability through tri-annual reviews. The hospital had to be operational for at least one year before it could be evaluated for accreditation by The Joint Commission.
It was time to draft and approve the articles of incorporation. The facility was recorded as a 501(c)(3) nonprofit hospital.
The Planning Begins
The pace quickened, and planning began in earnest. Three additional committees were created: the Bylaws Committee, with Chairman Leonard Robinson; the Building Committee, with Chairman Parvin E. Shaw; and the Fund Committee, with Chairman William T. Heseman.
In November, the bylaws were presented to a Citizens Committee for approval. The Barton Memorial Hospital Association was formed, and all individuals, businesses, and organizations that donated $200 to the fund drive were eligible to vote for the hospital board of directors. Members pledged $5 per month or more to join; for many donors, the commitment was based on 40 monthly pledges.
With board approval, the Building Committee appointed August W. Koenig as hospital consultant and architect to oversee the process, from starting discussions to opening day.
Meanwhile, architectural plans were designed by respected hospital architect John Badgley of San Luis Obispo, Calif. With its alpine flair, Badgley’s design reflected the mountain environment. Hospital size was set at 38 beds, or three beds per 1,000 residents, as suggested by the California Department of Public Health. The Incorporating Board also provided suggestions that would make the hospital expandable to 44 beds without additional construction. Rooms were planned for medical, surgical, pediatric, and maternity patients. Support services for dietary, housekeeping, maintenance, laboratory, and X-ray would also be housed within the hospital.
Under the direction of Lee DeLauer, fund-raising teams were created, each with a designated captain. George J. Wolf, C.P.A., was asked to serve as treasurer. Working under Fund Chairman Heseman were Walter Neal Olson, special gifts division chairman; Lloyd McBride, employees division chairman; Evelyn Heseman, employees division co-chairwoman; Robert W. Wood, absentee homeowners chairman; Glen D. Smith, public schools chairman; Henry Butler, business division chair-man; Glenora Bigelow, business division co-chairwoman; and Robert O’Mahoney, clubs and organizations chairman, who would later be joined by co-chairs Vic Gagni and Grace Schmidt. Residential oversight would fall to the Barton Memorial Hospital Women’s Auxiliary, provisionally led by Eleanor Gianotti.
The fund-raising kickoff, held at Harrah’s Club, was hosted by the Women’s Auxiliary with principal speaker Clifton Linville of Fresno Community Hospital. Badgley displayed his initial drawings. Fund Vice Chairman Vernon J. Wall, M.D., also president of the Lake Tahoe South Shore Chamber of Commerce, detailed the upcoming campaign. Public Relations Chairman William B. Ledbetter distributed campaign literature. Lt. B.B. Ball of the California Highway Patrol, who was in charge of the Lake Valley substation, affirmed the critical need for a local hospital.
Calculations showed that if each person on the South Shore contributed $50 to the campaign, the financial goal could be reached. Campaign slogans included “The Life You Save May Be Your Own,” “In an Emergency, Will Death Wait?” and “If You Care, Do Your Share.”
Gifts Large and Small
Heavenly Valley Ski Resort was the first business to pledge 100 percent participation on behalf of its five co-owners and 20 employees. Co-owner Chris Kuraisa pledged $3,000 to sponsor a precautionary nursery in memory of his son, Edward, who passed at a young age due to an accident. The managers and employees of Harvey’s Wagon Wheel dug deep to pledge a total of $91,692. The Rotary Club of South Lake Tahoe sponsored a patient room, and the Soroptimist International of South Lake Tahoe pledged to fund the admitting area. South Lake Tahoe Kiwanis members came in with a $2,000 memorial pledge. Safeway prided itself on 100 percent employee participation, which assured the purchase of a $200 Barton Memorial Hospital Association membership. In January 1961, the owners, management, and employees of Harrah’s Casino donated an incredible $24,000. Public school teachers pledged $9,000 to sponsor the dining room. Even tiny St. Theresa’s Parish school came up with donations totaling $50.10.
Creative fund-raising was at work. The first Lake Valley Firemen’s Association Ball divided its ticket proceeds (based on $1.25 per ticket) between the hospital drive and the firemen’s fund. Tahoe Valley Elementary School students raised $58 through a fashion and talent show. Girl Scout Troop 56 raised $20 through Christmas card sales. Local gas stations Orbit Stations and Tahoe Gasoline donated 10 cents per gallon of gas sold during a three-day sell-a-thon. The Tahoe Bowl bowling alley offered 15 cents off every line sold to the hospital campaign. Support came from all directions and in all sizes.
Support from outside communities brought more excitement—and more money. The San Francisco 49ers Cager basketball team, comprised of the 49ers’ professional football squad, came to Tahoe to compete against residents in a game coordinated by Bob Walker, South Tahoe High School basketball coach, with proceeds benefiting the campaign. Participating 49ers included Clyde Conner, R.C. Owens, Gordy Soltau, Bob St. Clair, Y.A. Tittle, and Billy Wilson. Hotel rooms for the players were donated to increase the contribution amount.
Fund-raising Breakdown
As of the February 8, 1962 Deadline
Special Gifts - $171,791
Businesses - $63,199
Employees - $103,732
Clubs and Organizations - $15,750
Seasonal Homeowners - $21,199
Residential - $16,317
Grants - $82,000
Total Raised by Deadline - $473,988
Crossing the Finish Line
Under the leadership of Chairwoman Eleanor Gianotti and Provisional Vice Chairwoman Betty Gay, the Women’s Auxiliary—now officially known as the Barton Memorial Hospital Auxiliary— hosted fund-raising events including the Christmas Tree Festival and Cocktail Party, the Winter Wonderland Fashion Show and Luncheon, the Headdress Ball, bake sales (with $3.50 cupcakes), teas, auctions, brunches, and even a communitywide stage play.
In January, the women created the Flying Squadron, making it easier than ever for community members to contribute. The group picked up and dropped off pledge cards and collected donations from residents, and raised more than $364,000 in less than three months. But the deadline to reach the $422,011 goal was just 13 days away. If hospital supporters did not meet that goal, all would be lost.
On February 1, campaigners got the miracle they needed. A gift of $82,000 upped the total funds to $473,988—beating the goal by $51,977. A hospital would now be a reality for South Lake Tahoe. This timely and generous gift came through a grant from the Max C. Fleischmann Foundation of Nevada. The foundation earmarked its support for the purchase of new equipment.
It was an exciting day for the people of the South Shore. But instead of stopping to cheer their success, they pressed on, continuing the momentum. Not one volunteer stopped fund-raising until the February 8 deadline. By the end of February, the final amount pledged or received totaled $605,000. It grew to $607,522 by November 1962, when the campaign was effectively over. The board of directors set aside the overage for landscaping, street paving, utility installation, and other items.
Tragedy and Triumph
Barton Memorial Hospital opened for business on Saturday, November 23, 1963. Though it was a big event for Lake Tahoe, a national tragedy cast a pall over the celebration. The day before, on Friday, November 22, President John Fitzgerald Kennedy had been assassinated in Dallas. Despite the devastation, Barton Memorial Hospital opened as planned, taking the first steps of a long and exciting journey.
MID- TO LATE 1960S - ALL ROADS LEAD TO BARTON

The 1960s were an exciting time at Lake Tahoe. The Lake Tahoe Airport, which opened in 1959, made access easier. As a result of the 1960 Winter Olympics at Squaw Valley, which showcased the region’s winter recreation, tourism began to grow. While skiing remained a big attraction and the casinos were flourishing, summer recreation also began to expand, with outdoor activities such as fishing, biking, hiking, and beach-going. Tourism population counts easily exceeded 70,000 per year. As industry grew, more people relocated to Tahoe, and both summer and winter seasons brought increased business to the hospital.
By 1965, when the city of South Lake Tahoe was incorporated, the year-round population had grown to more than 14,400 full-time residents. School enrollment on the South Shore rose from just 460 students in 1955 to 2,231 in 1960 and jumped to 4,432 by 1965.
For Barton Memorial Hospital, the timing was ideal. The hospital would be the medical provider for residents and visitors from the California west shore to the east shore at Glenbrook, Nevada.
The provisional board of directors looked to David Gay, nominating chairman, and his committee to come up with a list of 11 to 15 people to serve as the hospital’s first board of directors. They chose Lee DeLauer, president; David Gay, vice president and hospital equipment chairman; Elaine Kamp, secretary; George Wolf, treasurer and finance chairman; Robert Wood, public relations chairman; and Leonard Robinson, building chairman. The board was rounded out by members William B. Ledbetter, Henry Butler, Allen Mullen, Walter Neal Olson, and Thomas Regan, with terms ranging from one to three years. Because businesspeople did not have time during the workweek to attend volunteer meetings, the board met on the first Sunday of each month.
There was much to do. The first agenda covered clearing the land, planning for construction, and of course, more fund-raising. The to-do list was lengthy, and the pace would continue to accelerate.
Birth of the Snowflake
Architect August Koenig wanted to ensure that the mountain environment was represented in the 23,000-square-foot structure. Taking his inspiration from Lake Tahoe, Koenig incorporated heavy timber, stone, and glass in the design. The plan called for a central service area surrounded by pods for patient care. From above, the facility took on a snowflake look, which reflected the mountain aesthetic.
The cluster of pods, which were actually shaped like pentagons, was designed for optimum patient security and comfort. A centralized nurse station assured that a nurse was no more than 20 steps away from patients at all times.
By November 1961, the plans were finalized. In January 1962, Nomellini Construction Company of Stockton became the building contractor with a winning bid of $864,300, and pledged to begin construction as soon as weather permitted. The board made it clear that local workers were to be used as much as possible.
The 38-bed acute care hospital would consist of 26 medical/surgical beds with six private rooms and four pediatric rooms. Eight obstetrical beds would be housed in the maternity area. Also, an observation nursery would be constructed for babies born outside the hospital who were in need of additional checkups and newborn care follow-up. Cost breakdowns were $20,000 for medical imaging; $20,000 for the kitchen; $20,000 for each operating room; $15,000 for the nursery; $15,000 for a delivery room; and $4,000 for each patient room. Fortunately, many of these amenities were sponsored by generous donors.
Construction moved along, and the weather cooperated throughout the building season. By August, more than one-third of the exterior was completed. Interior construction would continue throughout the winter and spring. Over the years, as the hospital expanded, the original snowflake design would evolve and change. But the look was always unique to Barton Memorial Hospital.
Early in 1966, the hospital added a chapel, which later became a meditation room for visitors of all faiths. Decades later, it would be renamed the “family consultation/prayer room,” so physicians could have a private setting to speak with patients or their family members.
Growth, Evolution, and Controversy
In 1969, just six years after the hospital opened, two additional wings were approved by Administrator R.P. Hannum, expanding the Emergency Department, lab, Medical Imaging Department, and patient rooms. Hospital square footage increased from 23,000 to 46,000. The $2.9 million expansion, which opened in 1972, was funded by the sale of tax-exempt bonds. An additional 15 beds were added to the original 38. Laboratory and radiology grew. Soon, nuclear medicine was established with the purchase of the first CT (computed tomography) scanner.
Although the wings were built out, controversy ensued when the hospital tried to open the beds. California was strictly regulating new hospital beds at a time when growth was happening across the state. Although Barton Hospital could show the need for more beds on weekends and during seasonal peaks, a daily census did not confirm the need. The state said no more beds, but during the tourist season, the hallways were lined with patient gurneys. When the fire chief saw the situation, the hospital was cited for a violation of fire safety. That citation proved an effective counter-argument to the state’s position. Judge Terrence Finney ordered the beds open, and California complied.
Boom Time
At Barton Memorial Hospital in the early years, every physician was a family practice doctor, in theory. Even orthopedic surgeon Paul Fry II, M.D., delivered babies when the demand became overwhelming. Family practitioner James Whitely, M.D., delivered one baby after another during the latter part of the baby boom era.
By the end of 1966, 280 babies had been born at Barton, and other procedures were on the rise as well. During Barton’s first three years, more than 550 surgeries were performed, 7,327 X-rays were taken, and 16,427 lab procedures were conducted.
The emergency room was covered by every physician on the hospital medical staff on a rotating 24-hour call. Their specialties didn’t matter; emergency call was part of the job description.
The three emergency rooms averaged 35 to 40 cases daily. That patient load put quite a strain on the small department, especially in peak times, when the numbers escalated. Emergency visits totaled almost 8,700 in 1967. It was not uncommon to see patients filling the hallways on gurneys or even sitting on the floor as they awaited treatment.
Registered nurses and X-ray technicians were always available for emergency patients. Nurses performed triage assessments and administered patient care until the on-call physician arrived. Lab technicians often started IVs. In the absence of an anesthesiologist, a registered nurse served as nurse anesthetist. Even chief lab tech Ron Newton intubated patients as necessary. Everything was done by whoever had the knowledge and ability to assist.
In the late 1960s, Dr. Fry recalls that he counted 28 patients in the emergency hallway in a 24-hour period. With the help of Charles Hollingsworth, M.D., the doctors treated everyone. After 24 hours of nonstop work, they invited the surgery crew to Harvey’s Casino for a celebration breakfast before finally heading home.
Signs of the Times
Adoption
In the 1960s, babies born to unmarried mothers were commonly given up for adoption. Barton’s Maternity Department had a handwritten list of families eagerly awaiting the opportunity to adopt. The list was kept in a desk drawer, and as a mother neared her delivery time, families on the list were contacted and asked if they wanted the baby. A “yes” answer got them a call on the delivery date, and soon the baby was with a new family. After a trip to the courthouse and a home visit from the state, the adoption was complete.
Dual Licensure
In the early 1960s, Medicare did not exist; there were few insurance companies and much less government regulation. Because Barton Memorial Hospital was located along a state line, many physicians opted to become dual licensed in both California and Nevada. The process was simple. A California-licensed doctor could drive to Carson City, answer about 15 minutes worth of questions, and gain a Nevada license.
Ambulance Service
Fire Chief Parvin Shaw established himself as a one-man ambulance company, driving a modified station wagon for the purpose. Shaw fulfilled a vital service in the community until later selling to Warner Tooker, who maintained the service until 1968, when he sold to Les Bush, founder of Lake Tahoe Ambulance.
Have Blood, Will Travel
The California Highway Patrol (CHP) proved an invaluable hospital partner. As more surgeries were performed, more blood was required. The CHP frequently transported blood from the Sacramento Blood Bank to Barton Memorial Hospital. In cases in which a surgical patient needed extra blood, the hospital would send out the call by radio, asking for immediate donors of a specific blood type.
Administration, Accreditation
As hospital construction progressed, representatives of the California Nurses Association came to Tahoe to appeal for current and prospective nurses to join their organization. It was also time to start thinking about long-term, full-time leadership. The search for an administrator fell to the Hospital Personnel Committee chairman, Walter Neal Olson. Nearly 300 applications were received from across the country, and 50 applicants were invited to interview in Tahoe. Olson hired Frank Cook. Once hired, Cook had his work cut out for him, including the recruitment of 25 staff members for 16 departments. His campaign ended with the selection of 18 physicians and five dentists. Vendors were selected, equipment was purchased, and policies were developed. Cook would create the hospital’s first operational budget, which showed a projected loss for the first year. Long before Barton was eligible for accreditation, the hospital met all criteria for state and federal funding and, in 1966, earned its first passing scores from The Joint Commission, which accredits health care organizations in the United States. It has retained the accreditation ever since.
Seeds of Success
Early Orthopedic Care
Orthopedic surgery came to Tahoe in 1965, via the hospital’s first board certified physician, Paul Fry II, M.D. After serving in the military, Dr. Fry moved with his family to Tahoe to start an orthopedic practice. He recalls that it was a make-or-break deal for him. Not everyone on the medical staff welcomed him; some physicians felt there was not enough work to keep them all busy. But his colleagues soon acknowledged that Dr. Fry’s expertise could catapult hospital admissions and surgery volumes.
That expertise came at a personal cost to Dr. Fry. Although orthopedics was generating business, the hospital was not in a financial position to purchase equipment for the new surgeon. If Dr. Fry needed equipment, it would be up to him to buy it.
The early days of orthopedic care typically involved plaster casts. It was common for a patient to be casted and never be seen again by a physician for removal of the cast. Often patients simply wore the cast until it deteriorated to a point at which it could be torn off. The Rev. John Grace recalls wearing a leg cast for six long months, and he was not alone. With no workers’ compensation, sick leave, or disability coverage, people economized on health care to stretch their budgets.
With the heightened interest in alpine skiing after the 1960 Olympics, the ski industry boomed and the need for orthopedic surgery grew rapidly. Tahoe’s ski season usually started at Christmas time and could easily last into May. Once June arrived, the summer tourist season was in full swing and the orthopedic patient load would increase again.
In the Black
In the beginning, the hospital found it hard to meet payroll expenses. The solution came through short-term bank loans backed by board gifts and Auxiliary support, particularly from sales at The Attic Thrift Store. By the summer of 1964, the hospital marked its first month of operations in the black.
Patients typically paid their bills in cash, as insurance companies and Medicare were nonexistent at the time. In 1960, the average daily cost of hospitalization was $30; that grew to $65 by the end of the decade. With the significant increase in pricing, patients left the hospital as soon as they were able.
Some patients continued to barter for care. It was not uncommon to trade a cord of wood, side of beef, fresh fish, or other products for a physician’s services.
In 1967, the Barton Memorial Hospital Service Improvement Fund was established to fund and expand the Emergency Department from three rooms to nine. It was determined that if each of the community’s 5,000 households gave $10 each, the residential goal of $50,000 could be met. The Auxiliary had already committed $10,000 toward the $288,000 goal. The additional $233,000 was expected to come from part-time residents, grants, and large donors.
Barton Memorial Hospital was on the move.
1970S - THE CHANGING SHAPE OF BARTON
Life at Lake Tahoe changed following the opening of Barton Memorial Hospital. The community was growing in services, population, and activity. By the mid-1960s, the city of South Lake Tahoe had incorporated, and a housing boom followed. The Tahoe Keys development was complete, and more and more of its 1,500 homes were occupied by full-time residents. The population grew to approximately 7,500 year-round residents, and seasonal visitors brought an additional 100,000 people to enjoy the beauty of the area.
Hospital admissions increased from 1,698 to 3,702 patients in the first 10 years—an increase of 118 percent. During the same period, emergency room traffic rose 55 percent, from 5,785 annual visits to nearly 9,000. As the ski industry expanded, Lake Tahoe orthopedics also grew in reputation and prestige. Growth was evident as well at the snowflake-shaped hospital at the center of it all, as additions changed the pentagonal structure forever.
Patient Care
Laboratory
Laboratory business was steadily increasing. By 1970, 300 different blood tests were available on site—and more than 20,000 tests were performed annually. The three-member staff was busy and soon outgrew the small space. The lab was slated for improvements, with funding generated by the Hospital Service Improvement Fund Campaign.
Home Health
In the late 1970s, Barton Home Health Care was created in response to the rising cost of hospitalization. More patients were released from the hospital, with ongoing home care provided by licensed medical professionals. The concept carried into postpartum home visits, ensuring continuous care for both mom and baby.
Infection Control
Infection control became more important as more hospitals opened across the U.S. and more patients were treated. By the end of the decade, Barton assigned a full-time nurse to oversee the many aspects of infection, from prevention to follow-up care. Hand-washing became mandatory. Later, Annette Rhodes, infection control coordinator, would take charge of educational outreach regarding the newly discovered AIDS virus.
The Beginning of Managed Care
In 1973, President Richard M. Nixon approved the Health Maintenance Organization (HMO) Act. Managed care was created to fix pricing for patient care. From that time forward, Medicare reimbursements would be based on the minimum amount of hospitalization or medical treatment needed for a particular diagnosis. California Governor Ronald Reagan extended the same pricing structure to the Medi-Cal program. It was not long before insurance companies were negotiating for better rates and digging deeper into the “excess revenue funds” held by the hospital. The financial squeeze would be felt for decades and eventually lead to alliances between private practice physicians and hospitals nationwide.
Growth of Tahoe Orthopedics
In 1970, orthopedic surgeon Paul Fry II, M.D., was joined by revered practitioner Richard Steadman, M.D. Together the partners laid the groundwork for the Tahoe Fracture and Orthopedic Medical Clinic.
“Dr. Fry proved to be an exceptional partner, skilled as a surgeon and diagnostician with the highest ethical standards,” says Dr. Steadman. “The practice in Tahoe was busy from the first days.”
Soon after arriving in Tahoe, Dr. Steadman was asked to serve as a physician for the U.S. ski team. In 1976, he became chief physician for the team.
Soon, athletes from Europe and around the United States were seeking treatment at Tahoe. Champion skier and Olympic medalist Cindy Nelson was an early patient who came to Tahoe after suffering a serious ankle fracture in Europe. World Cup and Olympic stars Phil and Steve Mahre traveled to Tahoe for surgery, as did competitive skiers from around the world.
As the high-profile patients increased, athletes from other sports joined the throng, including Emil Boures, offensive lineman for the Pittsburgh Steelers, and Dan Marino, superstar quarterback for the Miami Dolphins.
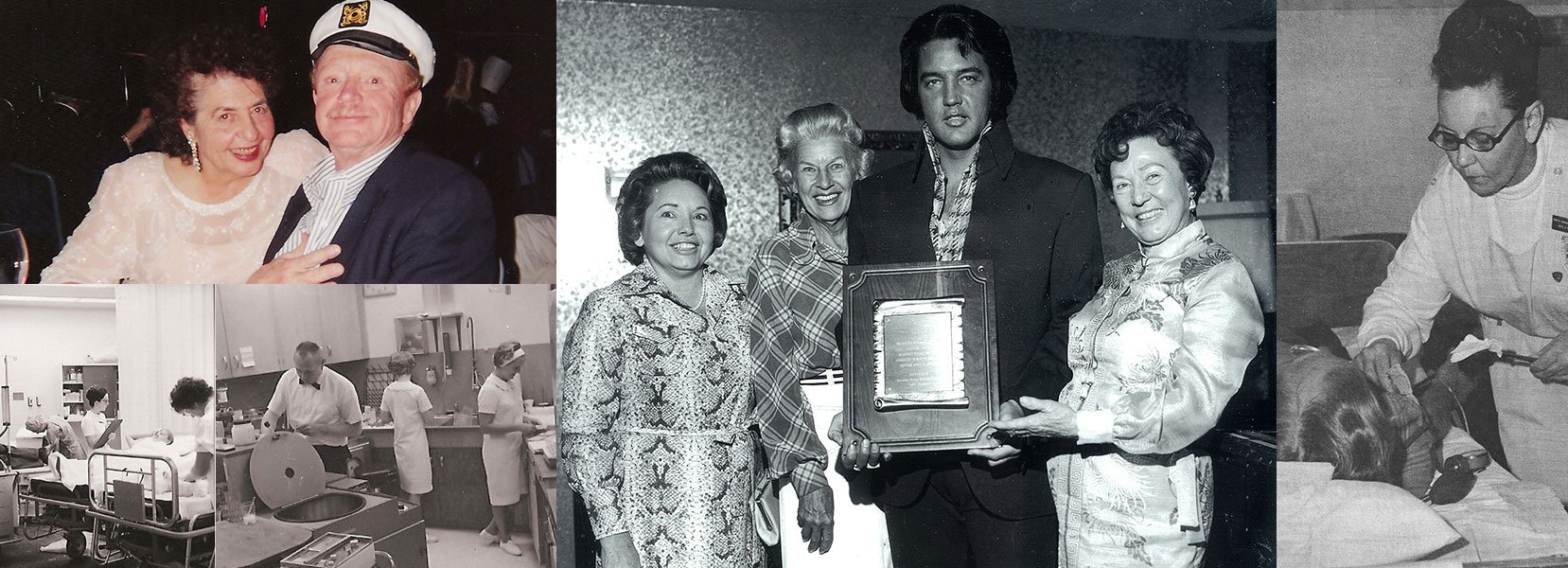
Gifts from the King
Over the life of an organization, there may be only a few instances that stand out as extraordinary. In Barton’s history, the 1960s fund-raising efforts came first. Global recognition for a stellar orthopedics program was another highlight, along with a growing roster of celebrity patients. Then came celebrity philanthropy, which linked Barton to some of the most famous names in entertainment history.
In 1973, Elvis Presley performed at Sahara Tahoe Casino in Stateline to a sold-out crowd. To thank Barton Memorial Hospital, where his late mother, Gladys, had once undergone orthopedic surgery with Dr. Fry, Elvis donated souvenirs and collectible items to the hospital Auxiliary. Martha Barneson, charter Auxiliary member, and her husband, John “Barney” Barneson, easily sold anything and everything that had been worn, touched, or owned by Elvis.
The King’s Mother’s Day performance, which he dedicated to Gladys Presley, generated an additional $12,000 for Barton. The concert revenue, along with more than $13,300 in souvenir sales, financed construction of the new Cardiac and Intensive Care wing, which opened in 1975.
1980S - LET THE GOOD TIMES ROLL

Throughout the 1980s, the focus at Barton Memorial Hospital was on the growth of medical services, continued community outreach, and sound financial planning. Physicians in many specialties joined the staff, and more patient services were introduced. Outside the hospital, the community was thriving. But it was also a tumultuous period for the hospital, marked by a nine-month strike.
Facilities Management
Barton Memorial Hospital
In 1980, to meet the rise in inpatient admissions, the California Department of Health licensed to Barton Memorial Hospital 19 additional acute care beds, bringing the total to 81. In 1985, the Laboratory, Radiology, and Surgery departments received capital funds for expansion. Nonclinical support services, including the business office, were moved off-site, reserving hospital space for patient care, support staff for that patient care, and administrative personnel.
With surgeries rising to more than 2,000 annually, the hospital added an additional surgical suite, bringing the total to three.
Barton Kingsbury Urgent Care Clinic
In 1983, Barton Kingsbury Urgent Care opened on the Nevada side of South Lake Tahoe. Nevada residents enjoyed having an urgent care facility close to their homes, but by 1990, the facility would close because of dwindling patient usage.
Patient Care
In 1980, new services were needed as the population grew. An in-house pharmacy and gastroenterology lab were added, along with ultrasound and computer axial tomography.
Gastroenterology
Until 1980, Henning Mehrens, M.D., handled all upper endoscopy procedures, but colonoscopies were not part of the services. When Dan Norman, M.D., joined the staff, he brought the gastroenterology board certification and specialized expertise not previously offered.
In 1985, Dr. Norman and Administrator Ronald Newton put their talents together in a successful redesign of 1860s instrumentation for hemorrhoid removal. After extensive testing, the instrumentation was patented in 1985, and in 1987, it was approved by the Food and Drug Administration. Called Ultroid, the device was then mass-produced by Boston Scientific.
Ambulatory Surgery
With the opportunity for patients to save up to 20 percent on the cost of their procedures, the addition of ambulatory surgery was a welcome improvement.
Education
In 1980, the Patient Education Department was created to benefit not only patients but clinicians and emergency agencies. In 1983, the department was renamed Education Services to better reflect its increased outreach. The program grew, adding courses for outside medical offices that included CPR, advanced cardiac life support (ACLS), childbirth preparation, and cesarean section education. Diabetes education took on enough importance to warrant its own department.
Discharge Planning
As federal regulations required more documentation, utilization review was created—a process in which nursing staff work with Social Services personnel to prepare patients for hospital discharge. Physicians were challenged by the new system, as it meant they would lose some control over patient care. The new protocol reflected the growing national view of health care as a business—weighing financial viability against the best patient outcome.
Pharmacy
Barton had operated for 17 years without an on-site pharmacy when The Joint Commission recommended the establishment of the service. Until this time, a drug room accessible only to lead nursing staff was stocked by outside contract pharmacists John Loeffler and Ron Renaldi. When the administration approached the men about setting up a hospital pharmacy, Renaldi designed the proposal and, with Doug Provan and Ron Thompson, gained approval for the contract. Thereafter, hospital pharmacists were responsible for all medications and narcotics within the hospital and ancillary facilities.
Barton Home Health Agency
Barton Home Health Agency was created in 1987 to provide a smooth transition for patients from hospital to rehabilitation to home. The agency received its first accreditation the following year and has passed all inspections since. Although this agency lost revenue over the years, the administration and board maintained that the service—which included nursing and respite care and various therapies—was critical for the community and would not be eliminated.
Companion Line
In 1987, the hospital Auxiliary funded the first companion phone line for high-risk patients living at home. Overseen by Home Health staff, the program grew over the years to accommodate demand.
Blood Drives
In the early days, the Auxiliary organized blood drives under the direction of member Pat Amundson, who was passionate about the program. Blood donors grew in number, and many achieved recognition for their giving. But as patients became concerned about possible tainted blood supplies, blood donations declined. Soon, more and more patients donated their own blood for upcoming ambulatory surgeries.
Endometrial Ablation
In 1989, the perception of hysterectomy as the solution of choice for women with gynecological problems was changing. A less invasive procedure known as endometrial ablation became the new version of the hysterectomy. The outpatient procedure used a Multifire Endo GIA—a combined surgical knife and stapler—in conjunction with a laparoscope, a tiny surgical telescope attached to a camera that guided the surgeon through the abdominal wall. The procedure was less traumatic, allowed for quicker recovery and lower costs, and provided effective outcomes.
Ambulance Service
In 1987, Curtis Weidmer, M.D., director of health services for El Dorado County, questioned the safety of Lake Tahoe Ambulance coverage based on standards of care and staff qualifications. After 19 years on the South Shore, Lake Tahoe Ambulance had its license suspended. West Slope Ambulance provided interim coverage, and services were later provided by Tahoe-Douglas Fire Protection District. For a year, the city and county tried to decide what the area needed, and when a grand jury report was finalized, Lake Tahoe Ambulance was back in business, on condition that two ambulances, staffed with EMTs, be available 24 hours a day. Later, the county board of supervisors changed the provider to Lake Valley Fire Protection in a service funded through property assessment fees.
Ultrasound
In 1988, Barton invested $180,000 in upgraded ultrasound technology. Mothers-to-be were able to view their babies in utero, and specialty physicians used the new technology for diagnostic tests. Ultrasound was also used in echocardiology care for patients requiring heart function tests.
Courier Services
At the end of the 1980s, the hospital purchased its first courier vehicle to pick up and deliver orders, specimens, and other products for the hospital, physician’s offices, clinical facilities, and off-site offices. This service significantly changed the turnaround time for lab results and communications within the medical community.
Executive Management
Computerization
Until the late 1980s, offices and staff at the hospital worked with typewriters and manual systems. With the conversion to automation and the start of the computer era, communications, processes, and patient tracking jumped light-years ahead.
Preferred Healthcare Network Provider
In 1987, Barton was selected as the regional orthopedic center for Preferred Healthcare Network in Reno. Patients could still go out of network for orthopedic surgery, but they would pay more out of pocket. The designation acknowledged Barton’s stature as a national and international leader in orthopedic care.
Within a few years, Barton designed a self-funded preferred provider organization (PPO) called Sierra Health Area Regional Partnership (SHARP).
The PPO signed on major employers in the South Lake Tahoe basin for contracted medical services. Soon afterward, SHARP was dissolved, and competition increased in the HMO and PPO businesses.
Community Outreach
In the 1980s, community outreach, education, and training programs blossomed. Flu immunization clinics were held along with support groups such as Smoke Stoppers. Physicians joined the movement and presented health-related lectures and free screenings.
In 1986, St. Theresa’s Parish Hall started hosting community health fairs, and Barton participated with laboratory blood panels and other wellness tests. Over the years, the events and venues would change, but the outreach efforts continued to provide valuable medical information and access through Latino health fairs, women’s wellness days, health care lectures, community event presence, and reduced price screenings, among other beneficial programs.
Strategic Planning
In 1987, hospital officials finalized a nine-point plan designed to enhance the hospital’s community image, create joint ventures with physicians, establish a skilled nursing facility, research options for substance abuse treatments, cultivate managed care relationships, develop ambulatory surgery, design wellness programs, purchase an MRI (magnetic resonance imaging) machine, and expand the Physical Medicine and Rehabilitation Services.
Financial Management
In the late 1980s, physicians and hospitals across the country experienced a financial squeeze as the cost of medical care rose and reimbursement fell. At the time, Medicare paid just 49 cents on each dollar billed, and Medi-Cal only 55 cents. Barton’s response was to hold off on capital improvements, freeze hiring, cut staff through attrition, and restructure for efficiency. Operational efficiencies were evaluated and adjustments made to meet lower staff requirements. All nonessential purchases were deferred.
A nationwide nursing shortage added to the rising cost of health care. Nursing registry personnel were brought in for busy periods, and employment rates increased significantly. Higher salaries—along with rising debt, an increase in high-tech equipment costs, more discounted insurance programs, and the decrease in federal and state reimbursements—contributed to a gloomy financial outlook for hospitals.
CEO William Gordon and new Chief Financial Officer Margaret Lera teamed up to prepare a financial analysis, cutting costs and staff where possible. Their prudence put the hospital on sound financial footing as the decade drew to a close.
The Strike of 1986–1987
Communication doesn’t always prevent problems, so when a wage and benefits dispute arose at Barton, a group of hospital employees sought union representation. In 1986, a labor strike led to a board recall attempt and the eventual departure of Administrator Ronald Newton. Employees were dissatisfied with their compensation and benefits package, and when the board of directors voted for a stipend of $500 per board member per month, it eroded the trust once shared by employees and the board. Times were turbulent at Barton.
But in 1987, everything changed. A generous employee benefits package included raises averaging 6.6 percent for all employees and the promise of annual reviews. The new-hire probationary period was reduced to three months, and a retirement package was developed. The board rescinded the monthly stipend, the strike ended, and workers returned to their jobs. The union was voted out at that time.
The Summit of Orthopedic Care
When professional athletes came to Barton Memorial Hospital, they turned heads like casino headliners.
With the growing interest in orthopedics, the early 1980s saw the launch of Tahoe’s Sports Medicine Fellowship. Richard Steadman, M.D., had begun a program that would spark international interest. However, after a couple of years, the program waned, largely due to the tremendous patient volumes requiring Dr. Steadman’s attention. By 1984, Randy Watson, M.D., took the lead to create the Lake Tahoe Medical Fellowship.
That fellowship—which began as a six-month program and later grew to a yearlong course of study—attracted participants from around the globe. In addition to Dr. Watson, the faculty included Keith Swanson, M.D., and Edward Tapper, M.D. Scott Southard, M.D., and Terrance Orr, M.D., became Tahoe Fracture Clinic partners participating in the fellowship program.
In 1988, Dr. Steadman founded the nonprofit Steadman Sports Medicine Research Foundation at Tahoe and, in 1990, relocated his practice to Vail, Colo. “I have wonderful memories of the great care provided by the staff of Barton Memorial Hospital during my time in Tahoe,” says Dr. Steadman.
The loss of the eminent physician was expected to be keenly felt at Barton. However, the orthopedic surgeons remaining on staff went on to implement and develop other successful procedures, and they remain front-runners in orthopedics today.
Together, this group of physicians earned worldwide renown, including Dr. Orr, who was acclaimed for his nontraditional ACL repairs, and Dr. Watson, who became well known for his successful shoulder surgeries. Like Dr. Steadman, Dr. Watson worked with the U.S. ski team, and a significant amount of his business came from those world-class athletes. Dr. Watson recalls off-season trips to glaciers where the team would train year-round. After morning ski runs, the glaciers would become makeshift football fields. The relationships built in those years increased referrals to Tahoe Fracture Clinic.
Among the techniques advanced at Barton was arthroscopic surgery, which uses a video camera for diagnostic and operative surgery. Surgeons at Barton stayed ahead of the curve with this surgical technique. According to Dr. Keith Swanson, it was “a major advancement in orthopedic technology” with many benefits, including early ambulation, reduced postoperative discomfort, minimal scarring, and shorter hospital stays. Stephen Abelow, M.D., Barton orthopedic surgeon, hailed the use of the CTi derotation brace, which reduces recovery time. “A mild electronic stimulus helps prevent loss of muscle mass and has pain-relieving properties,” he says.
In 1986, the introduction of continuous passive motion equipment brought rehabilitation to the next level and increased recovery rates. During the procedure, the patient’s injured limb would be secured in the equipment. It would then be moved slowly and continuously for up to 20 hours per day to boost mobility and muscle tone.
Star Power
In 1981, celebrities were a big draw in Lake Tahoe. Bette Midler came to Harrah’s Lake Tahoe to film the movie Jinxed, and the production company decided to contribute to a local charity. Harrah’s CEO, Tom Yturbide, encouraged support for the hospital. Midler presented a check for $10,000 to Barton Hospital Auxiliary, a contribution that funded the hospital’s first birthing suite. That same year, entertainer Jack Ross, headlining at Sahara Tahoe, presented a $5,000 check to the hospital after performing at a charitable auction for the Jack Ross Dialysis Classic Golf Tournament.
A short-lived TV series and a TV movie were filmed at the hospital itself. The 1987 series was High Mountain Rangers, with Robert Conrad and the 2005 movie was Out of the Woods, with Ed Asner. Several employees made their television debuts working as extras.
1990S - REDEFINING HEALTH CARE FOR LAKE TAHOE

In the late 1980s and early 1990s, health care underwent unprecedented changes as hospitals opened and closed, downsized and supersized. Nursing shortages came and went. And Barton Memorial Hospital needed a face-lift. Its successful growth during this era is evidenced by the facilities that now make up Barton Health. The 1990s emphasized outpatient services, facility improvements, and physician recruitment.
Patient Care
Laser Technology
In 1990, equipment was being developed to help revolutionize surgery. Laser technology at varying wavelengths enabled cleaner, more efficient surgical procedures. The new technology resulted in reduced blood loss, scarring, pain, and recovery time.
Occupational Health
Occupational Health opened to provide businesses with workers’ compensation patient care, pre-employment drug screenings and physicals, ergonomic evaluations of work stations, Occupational Safety and Health Administration training, immunization programs, and more. Employers now had a partner in their employees’ health and wellness. This service continued to develop as employers sought to keep medical costs down and reduce work time lost due to injuries.
Medical Imaging
The $2.3 million expansion of the Medical Imaging Department was finalized in 1991. The 2,000-square-foot renovation introduced state-of-the-art CT scan technology for more precise patient diagnoses. Additional improvements included a gamma camera for diagnostic tests and an angiogram suite. Imaging services were enhanced by the purchase of the first mammography equipment for an outpatient facility.
Neurology
In 1991, neurologist Michael Sullivan, M.D., brought a first-time service to Tahoe. Dr. Sullivan gained expertise in acute mountain sickness, or altitude sickness, when he studied in the Himalayas and served as the primary physician for Mount Everest climbers. Sullivan offered welcome services for those with high-altitude health issues. No longer would patients requiring neurological treatment have to travel off the hill.
Nursing
In 1994, the staff-to-patient ratio for acute care patients was one nurse plus an aide for every six to eight patients. This “team nursing” concept was an improvement over the previous ratio of one nurse for up to 12 patients. With the team approach, nurses could concentrate on nursing while aides provided support.
Meanwhile, new opportunities abounded in the nursing field. Nurse practitioners shared routine care duties under the direction of a physician, making patient care more efficient and cost-effective. Patty Bucher was the first nurse practitioner in Tahoe, sponsored by Tahoe Family Physicians.
Birthing Centers
In 1998, many hospitals transformed maternity suites into birthing centers. No longer did traditional births take place in one room with recovery in another. The mother, along with her partner or coach, could have a private room for labor, delivery, recovery, and postpartum. The baby could remain in Mom’s room unless medical conditions dictated otherwise.
Bone Density Testing
In 1999, the first densitometer was purchased for Tahoe Family Physicians. As the population aged and women’s health became a significant market for medical care, the purchase was prudent. Osteoporosis and other related conditions could be identified quickly, and physicians could create personal prevention or treatment plans in a timely manner.
Hospice
Barton Home Health Agency had been serving the Carson Valley since 1993, but it wasn’t until 1997 that Hospice of the Lake and Valley received licensure to serve the population from Lake Tahoe to the outlying areas of Dayton, Nevada, and Walker, California. Terminally ill patients were able to remain at home and receive compassionate, quality care from hospice clinicians. With the majority of patients on Medicare or Medicaid, reimbursement did not cover the cost of doing business. Financial concerns, as well as the knowledge that competitors were covering the area, led to the closing of the Carson Valley coverage in late 2011. However, hospice services in Lake Tahoe continue.
Orthopedics
Competition from the new Lake Tahoe Surgery Center in Round Hill adversely affected hospital surgeries for a period of time, but Tahoe Fracture Clinic remained busy.
In 1992, Michael Fry, M.D., joined the clinical staff. His expertise in sports medicine for the back and spine added a new specialty service for the Lake Tahoe region and brought in new patients. In 1997, Stephen Bannar, M.D., joined the orthopedic staff.
Barton-Incline Urgent Care
When Incline Village Hospital closed in April 1991, Barton’s administration saw the opportunity to provide urgent care services to an underserved population. Many Incline Village physicians encouraged Barton to purchase the hospital. While a purchase was not in the plan, Barton Memorial Hospital and Elliott Schmerler, M.D., an Incline Village family practice physician, partnered to create an urgent care center that operated for three years. The doors closed only when Lake Tahoe Medical Center reopened in Stateline, filling the void in care it had left several years earlier.
Barton Clinic at Kirkwood Mountain Resort
During the 1980s, Tahoe Fracture Clinic had contracted for medical coverage on the slopes of Kirkwood Mountain Resort. By 1991, it handed the coverage to Barton Hospital. The hospital purchased the equipment and established Barton Clinic at Kirkwood for all urgent care needs during the winter. With almost 900 patients treated in the first season, the clinic proved a valuable addition to both the hospital and the resort. It operated for several years before the resort assumed management of the facility, and it returned to Barton management in 2012.
Executive Management
Board of Directors in the 1990s
Board members are elected for three-year terms by the Barton Memorial Hospital Association. The board consists of 10 elected members and four ex officio members—a chief of staff, auxiliary president, foundation chairperson, and hospital administrator. The time commitment for board members easily ranges from 60 to 100 hours every month. In return for their investment of time and expertise, group health insurance is offered at a minimal cost—a small price to pay for the benefits the hospital receives.
Proactive governance starts at the top. The board and executive team attend annual conferences to learn about health care trends, hot issues, and new opportunities. They continually evaluate ways to reduce hospital stays, cut costs, improve services, and enhance the value of the corporation's investments. The ultimate responsibility of a solid, strong hospital rests on the shoulders of its board.
No Sale
For years, speculation circulated that Barton would be sold to Sacramento hospital conglomerate Sutter Health. To ease staff concerns and set the record straight, CEO William Gordon invited Sutter Health CEO Pat Fry to a public presentation at Barton. Fry conceded that Sutter was interested; if Barton’s board of directors wanted to entertain a sale, Sutter would be at the front door. But the board made it clear that the hospital would remain independent to keep decisions local and guide the direction of future growth. The rumor mill was silenced.
Computerization
As the decade rolled on, computers took over. Each department in the hospital wanted software specific to its area of expertise: patient care, financial management, support services, personnel administration, and beyond. By the end of 1999, 81 electronic servers were in place to process information for Barton.
Pay for Call
Until the 1990s, physicians were required to be on call for the Emergency Department. They were not paid for their time and expertise—it was simply a condition of staff credentialing. Barton decided to follow the national trend of compensating physicians and the “pay for call” model was established.
Education
In 1992, the Technician Assistant Training Program was founded. The summer training program enabled graduating students from Whittell and South Tahoe high schools to train in multiple areas of the hospital. After 160 hours of clinical rotations, it was expected that students would have confirmed their passion for health care or opted for other careers.
Financial Management
In 1998, shortly after the Lake Tahoe Surgery Center opened, Barton CEO William Gordon projected a loss of $5 million to $10 million in ambulatory surgery revenues at Barton Memorial Hospital. At the time, ambulatory surgery generated approximately $90 million in annual gross revenue; Barton would be hard hit by the loss.
That anticipated shortfall came on the heels of the Balanced Budget Act of 1997, which called for a 16 percent reduction in reimbursement for Medicare patients. Services that were previously covered now were off the Medicare plan.
Operating on a $58 million budget in 1997, Barton Memorial Hospital ranked 66th in revenues among the largest 100 private companies in the Sacramento region. Barton showed revenues of $50.6 million, a 14.2 percent increase over 1996, when the hospital ranked 79th. After expenses, about $4 million was available for reinvesting in facilities and technology.
Gordon indicated the increase in revenues was due largely to the opening of the Skilled Nursing Facility (SNF) and the growth of CVMC, which had seen 30 percent annual growth since it opened four years earlier. CVMC gave the Barton Health System expansion opportunities when growth at the lake was not expected. Likewise, the SNF provided a vital service that maintained high occupancy and generated revenue.
Although the hospital’s financial outlook was fairly stable in the 1990s, cost containment remained a big issue. Despite the decline in ambulatory surgeries, the procedures continued to generate revenues—and raves. The surgeries reduced the use of beds, rooms, and other amenities that come with inpatient services. Insurance companies promoted the idea, and hospitals received better reimbursements. Patients, too, preferred one-day surgical procedures, which allowed them to recover in the comfort of their own homes.
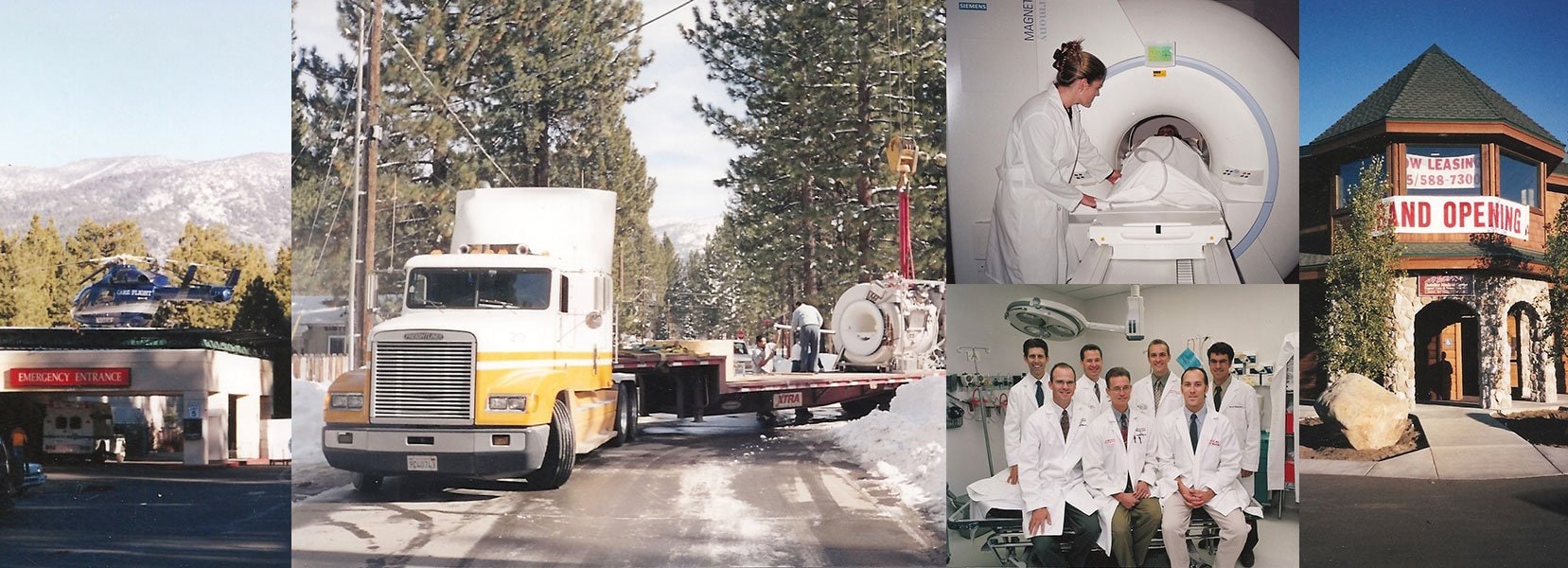
Giant Steps: Barton Grows Again
By 1992, Barton Memorial Hospital had grown beyond a small community hospital. Groundbreaking for an additional 60,000 square feet of hospital space took place on May 27, 1993. The expansion, which was complete in 1995, increased space in the overcrowded Emergency Department and added two additional surgical suites, for a total of five. Additional drawings included space for the growing outpatient service sector.
As services moved from the original hospital, 48 patient rooms were renovated to introduce long-term nursing care to Lake Tahoe. The Maternity Department grew to five private birthing suites and three semiprivate rooms. Improvements were also made to physical therapy, occupational therapy, speech therapy, neurophysiology, gastroenterology, and EKG/ECG. Financing for the $15 million project came from the sale of tax-exempt bonds enhanced by fund-raising efforts by the Barton Memorial Hospital Foundation. $2 million of the financing was earmarked to pay off the 1978 bond.
Laboratory
In 1998, the final section of the original “snowflake” construction disappeared when the laboratory doubled in size to accommodate the 300,000 tests conducted there each year. A satellite laboratory was established at Stateline Center in Nevada to better serve Nevada patients.
Carson Valley Medical Center (CVMC)
After years of watching the Carson Valley, Nevada, towns of Gardnerville and Minden grow in population, Barton officials considered building an outpatient facility there. Family practice physicians in the Valley were enthusiastic about the plan. A 10-acre plot was purchased for a new facility, with room for future expansion. The first phase cost $3.8 million and was contracted to the Hospital Building and Equipment Company, the same contractor that completed Barton Memorial Hospital’s expansion.
In 1994, Carson Valley Medical Center (CVMC) opened with 28,000 square feet of outpatient services. The facility offered physician offices, a laboratory, physical therapy, cardiac rehabilitation, pharmacy, radiology, home health, and hospice services to a previously underserved area. Barton Chief Executive Officer William Gordon would tout this as the most successful venture under his leadership.
CVMC CEO Michael Luckin worked diligently on physician recruitment with Lake Tahoe doctors who wanted to enlist new patients. For the first few years of operations, the Barton management team oversaw all areas. Growth within the first year kicked the second phase into action: the construction of an urgent care clinic and ambulatory surgery unit. Soon, the part-time urgent care facility grew to full-time emergency care with a helipad for timely patient transfers.
By the late 1990s, patient demand confirmed the need for a hospital in the Carson Valley. To provide the best patient care technology, CVMC purchased a multislice CT scanner, MRI scanner, and telemetry unit.
Tahoe Family Physicians
Tahoe Family Physicians (TFP), which opened in 1981, grew into a large-volume practice with obstetrics, pediatrics, and geriatrics, in addition to family care, and filled a void in care for Medi-Cal patients. In 1989, the TFP doctors opened the El Dorado Community Clinic, which served as a catchall for the uninsured and underinsured. Patients received evaluation and diagnosis by a physician assistant or nurse practitioner working under a TFP physician. Fees were determined by a sliding scale based on income.
By the mid-1990s, TFP became the first physician group to contract with Barton for management services, enabling the physicians to focus exclusively on patient care. Shortly thereafter, the partners—Greg Bergner, M.D.; Brooks Martin, M.D.; and Paul Rork, M.D.—sold the practice to the hospital. All three joined Tahoe Carson Valley Medical Group (TCVMG) to continue practicing medicine. Drs. Bergner and Rork later moved to Barton Urgent Care. Dr. Martin stayed with TFP, recruiting a new generation of doctors and growing a vibrant practice.
Job’s Peak Medical Group
As trends in health care evolved in the mid-1990s, so did Barton’s ownership and management of physician practices. Job’s Peak Primary Care focused on pediatrics and internal medicine. Both specialty areas grew rapidly and expanded from Lake Tahoe to the Carson Valley. In the following decade, separate identities were developed for the evolving Job’s Peak Pediatrics and Job’s Peak Internal Medicine, both in Tahoe and Carson Valley.
Barton’s Management Services Organization (MSO)
Barton’s Management Services Organization (MSO) was created in 1996 to meet the needs of local physician offices. The organization offered oversight for office support, management, accounts receivable and payable, payroll, and collections. By using the economy of scale, physician offices could reduce their overhead costs while maximizing their office efficiency.
Barton Community Clinic
By 1995, Barton and Tahoe Family Physicians agreed that the hospital would assume the clinic services. The clinic continues to operate under the name of Barton Community Clinic, and the scope of services and treatment has expanded. Specialty physicians provide their expertise on an ongoing basis, and more staff has been added to meet growing demand.
Barton Skilled Nursing And Rehabilitation Facility
Until the late 1990s, residents had to travel to Carson Valley and beyond to find long-term care facilities. Barton Skilled Nursing (SNF) opened in Tahoe in 1998 with 33 beds for extended care and 15 for rehabilitation. The SNF filled a long-standing need in the community and provided better continuity of care for people in need.
Virginia Creek Skilled Nursing Facility
Virginia Creek Skilled Nursing Facility, located behind CVMC, offered independent assisted living along with a program for patients with Alzheimer’s disease. In 1988, the facility contracted with Barton for management and clinical staff. But the facility was operating at a loss, and after almost four years, the financial undertow brought the business to an abrupt end. Residents were quickly relocated, and the facility closed in 1992.
2000s - BIG CITY TECHNOLOGY, SMALL-TOWN CARING
Over the past 50 years, patient needs and demands have changed dramatically. Just think back to 1947, when the average hospital stay was 13 days. As of 2013, the average stay was only three and a half days. The inpatient census dropped during the first decade of the 21st century, leading to a reduction in licensed hospital beds and a surge of outpatient services. Patients had more treatment options, and hospitalization wasn’t necessarily the right or only answer. People became actively involved in managing their own health. Fifty years ago, it was typical for one physician to tend to all of a patient’s medical needs. Today, patients can have several doctors overseeing different aspects of their care.
Patient Care
Barton Health Resource Center
Barton Health Resource Center opened in 2001 to meet the public’s demand for more information about health care. The center provided a resource library of periodicals, journals, reference manuals, videos, and more. Support groups and other organizations used the center to reach community members and market their programs. Over a six-year span, the center had its finger on the pulse of the community. As more people gained access to computers and the hospital website offered medical research tools, the responsibilities of the resource center changed. Additional outreach components were eventually shifted to become a part of Barton University and the hospital's Public Relations department.
Infusion Center
In 2004, the hospital’s Infusion Center opened, enabling cancer patients to remain in Tahoe for therapy and treatment in a reassuring environment that included comfortable recliners, warm healing colors, and trained, compassionate staff. The service had begun in 1993 as the Home Health Agency’s Home Infusion Therapy.
Sleep Studies
Sleep studies were introduced in 2005 to address a growing medical concern. Overnight accommodations, trained staff, and technology all provided the right mix to evaluate patients in a realistic setting. Extensive studies and monitoring allowed clinicians to offer a treatment plan for each individual.
Barton University
Barton University was established in 2006 as a comprehensive learning center for clinicians in the Lake Tahoe Basin, as well as a resource for Barton Health employees in search of continuing education. Medical professionals and allied health workers were now able to complete Web-based training for required courses on their own time. Translation, interpretation, and signing services for patients were incorporated into a formal program. Barton University now offers customized classes for regional businesses and organizations to help them meet workplace safety, health, and wellness training needs. It also holds several national symposiums for continued Medi-Cal education.
Medical Imaging
Until 2001, when Barton purchased its first MRI machine, medical imaging services were provided by a private physician group nearby. Tahoe Imaging Center operated independently until the MRI was purchased and relocated to the hospital. By 2007, the MRI was upgraded to an Achieva 1.5T with three-dimensional capabilities. The noninvasive, painless procedure and enhanced imagery helped physicians diagnose many conditions including cancer, heart and vascular disease, stroke, and joint and musculoskeletal disorders.
A picture archiving and communication system (PACS) was installed to offer filmless radiology for reports, X-rays, and scans. By converting to electronic reports, anyone with access privileges could view the results instantly, greatly increasing physicians’ abilities to determine the best treatment for their patients and communicate the information in a timely manner.
The Brilliance 64-slice CT scanner offered unprecedented diagnostics to Barton clinicians. The technology provided higher resolution and expanded clinical boundaries in cardiac imaging, pulmonary imaging, brain perfusion for stroke assessment, and CT angiography.
In 2007, digital mammography was introduced at Barton. Radiologists were also able to start performing heart scans and kyphoplasty. Technology continued to improve for both patient and physician.
For a time, the common approach to dealing with varicose veins was to strip the rope-like veins in patients’ legs. The less invasive endovenous ablation procedure was touted by the Mayo Clinic as the “best technology available.” Acquisition of the Diomed endovenous laser treatment provided Barton radiologists a better solution for patients with varicose veins.
Surgery
Surgical suites went digital and incorporated the latest high-definition video system for minimally invasive surgery. Surgeons could make small incisions and use an endoscope to view the operation on a video monitor. With 1,100 such surgeries performed annually at Barton, the investment was a wise one. The surgical suites became fully integrated digital endosuites with LED lights and high-definition cameras. New technology reduced operative time, decreased recovery time, provided a more ergonomically friendly environment for the staff, and created a shorter anesthesia period for the patient. Electronic patient records could be viewed in the surgical suites, enhancing patient care, especially for trauma victims.
Gastroenterology
By the new millennium, the GI Lab, which opened in 1980, had grown to 1,300 square feet with two operative suites and six staff members. Colonoscopies and other GI procedures have grown to more than 1,600 procedures annually. An advance added in 2011 is colon hydrotherapy, an alternative for patients who cannot tolerate standard preps for colonoscopies. Barton Memorial Hospital is still one of the only hospitals in the nation to offer colon hydrotherapy as a preparatory method for patients.
Pharmacy
In 2003, the Barton Auxiliary purchased the medication-dispensing cart system Pyxis, which enables pharmacists to track individual dosages and maintain a more secure and accurate distribution method.
TeleHealth Technology
In the late 2000s, Barton introduced TeleHealth, a high-definition, high-quality video and audio system that enables local physicians and patients to connect with specialists remotely in a seamless exchange of information. Patients can remain in Tahoe for a thorough evaluation while consulting physicians collaborate to determine the next steps. Expanded telemedicine services and specialty physicians have brought new expertise to Tahoe patients with the help of a grant from Access El Dorado. Through the leadership of Telemedicine Coordinator Ann Truscott and Physician Leader Gregory Bergner, M.D., the grant funded new equipment for endocrinology, adult psychiatry, cardiology, neurology, dermatology, nephrology, and medical-surgical intensivists. This high-tech medical specialty access, from Lake Tahoe to specialists at top health care institutions, transitioned Barton Health to a rural leader of choice. The interactive video gives outside specialty physicians a direct connection to local patients while the patients remain in their hometown. In 2012, the chairman of the Federal Communications Commission (FCC), Julius Genachowski, visited Barton Memorial Hospital to see the success of this program, which advances health care delivery, especially in rural areas such as the Lake Tahoe region.
Epic
In 2012, Barton Health started using the Epic electronic medical record. Until 2012, physician offices, departments, and the hospital used best-of-breed technology that interfaced but did not interact seamlessly. Large health systems such as the Cleveland Clinic, UC Davis, and Stanford University Hospital use the Epic system to help improve communications between health facilities, facilitate fewer errors, reduce costs for health systems and their patients, and create a better continuum of care for patients regardless of where they go for care. Barton’s partnership with Renown allowed Barton to implement this advanced system, one of the most expensive capital investments in the history of Barton, exceeding $7 million in equipment, training, and software.
This integrated health record system will enable Barton to not only improve patient care, but also improve efficiencies and satisfy federal electronic medical record mandates.
Patient Safety
Continuous quality improvement (CQI) processes are monitored for all hospital areas. As Barton moves into the value-based performance pay regime established by Medicare for reimbursement in 2012, oversight and patient outcomes become more critical. As Medical Staff Officer Clint Purvance, M.D., observes, “It’s all about developing the right care for the right patient at the right time.” CEO John Williams confirms that quality is just as critical as financial performance. Barton believes so strongly in the success of the patient safety initiative that an entire department has been created to monitor and provide oversight for safety issues.
Level III Trauma Center
Barton Memorial Hospital is moving toward accreditation for a level III trauma designation in 2013. Emergency staff is receiving training in specialized trauma treatment, coordinated efforts with medical partners, and heightened preparedness to save lives. Barton Trauma Center will offer 24-hour ER, 24-hour anesthesiology, and 24-hour general surgeon coverage, as well as other significant process improvements to enhance the care of trauma patients.
Additional evaluations were performed on systems for efficiency, safety, quality, and care. As transparency permeates the medical community, aggregated patient outcomes are posted on the Web for easy reference. With the level III trauma center designation, additional county funds have helped support Barton Memorial Hospital in maintaining higher standards.
Physician Recruitment
In 2006, the hospitalist program was expanded to include eight internal medicine physicians. Primary care physicians have the option to refer inpatients to a hospitalist or to monitor their patients personally. Hospitalists maintain their continuing education exclusively for this level of care and bring another layer of expertise to these patients. This program has also helped reduce patient days in the hospital. In 2011, Barton recruited an audiologist and cardiologist, along with a physiatrist from the Mayo Clinic to add expertise in non-surgical sports medicine care and concussion management.
Da Vinci Robot
In 2012, the use of robotics in urology, gynecology, and general surgery was the gold standard in care. Barton purchased the da Vinci robotic surgical system at a cost of $2 million. Robotic surgery allows minimally invasive techniques that result in improved patient outcomes, shorter hospital stays, fewer anesthesia minutes, fewer blood transfusions, fewer narcotics, less need for pain control, and decreased recovery times. Barton Memorial Hospital, through this purchase, became one of the first hospitals in the region to offer single-site surgery with this technology, again placing Barton at the forefront of rural hospitals in the nation.
Facilities Improvement
The Barton Mountain Café
In 2003, improvement of the Dietary Department reached the top of the to-do list. The $4 million remodeled cafeteria and kitchen added 10,000 square feet to one side of the hospital’s remaining snowflake design. Finally, employees, visitors, and even patients could enjoy a spacious, comfortable dining experience in the new Barton Mountain Café. The patio and barbecue area feature outside seating surrounded by water features and landscaping. Due to the fine food and improved environment, the Barton Mountain Café won “Best of Tahoe” awards from the local community and readers of the Tahoe Tribune three years in a row, 2008 through 2010, as the best food for less than $5 in the area.
The new physician dining room—long overdue and greatly appreciated—features an executive table, flat-screen television, and digital technology, replacing the old no-frills break room with its collapsible tables.
The original hospital was also upgraded to comply with new regulations for earthquake safety and retrofitted to higher seismic safety standards.
Rehabilitation Expansion
The Rehabilitation Department received a massive overhaul in 2009. The $2.8 million project expanded the tight space from 740 square feet to an impressive 6,000 square feet. Highlights of the new space includes a therapeutic hydrowave pool, which has proven to reduce patient recovery times. The department also includes ample space for hand and speech therapies; an orthopedic fellowship room for research and training; a gym with free- and fixed weights; three private exam rooms; and ancillary support services, all in a warm, inviting, Tahoe-esque environment.
Barton Health Family Birthing Center
In 2009, the upgraded Family Birthing Suites, funded through a generous gift from Ethelmae Haldan, introduced large, private, redecorated suites for labor, birth, and postpartum time. The most up-to-date birthing equipment and upgrades, including televisions, DVD players, and wireless Internet access, helped provide homelike comforts for a more enjoyable stay.
Carson Valley Medical Center (CVMC)
In 2000, Barton Memorial Hospital found a new partner and partial owner of Carson Valley Medical Center. In November, an agreement was reached between Barton HealthCare System and Washoe Health System (later Renown Health) for a 50-50 partnership. Barton’s decision to sell was based largely on the hospital’s difficult financial position. Funding was needed for capital improvements for both Barton Memorial Hospital and CVMC. An influx of cash would provide resources for additional services, new equipment and technology, the recruitment of more top-notch physicians, and other capital improvements. The partnership changed many aspects of the operation, starting with a board that would represent both organizations equally.
In 2004, CVMC was approved for licensure as a Critical Access Hospital (CAH) with 15 acute care beds. This status allowed for reimbursements based on cost plus 1 percent, significantly higher than the acute care settings established by Medicare. In most cases, patients in the Carson Valley area were able to stay in their hometown for up to 96 hours of hospitalization. With the transition to a hospital, the facility upgraded both computerized tomography (CT) and magnetic resonance imaging (MRI). New medical imaging technology also included mammography and ultrasound equipment. Additional ancillary services were increased to provide full service for the hospital. The construction project was financed through $7.7 million in tax-exempt bonds.
While CVMC was experiencing growth, another 31 acres of land adjacent to the center was purchased for possible future expansion.
Stateline Medical Center
In 2000, officials at Barton HealthCare System acquired Rebecca Rezaei, M.D.’s Zephyr Medical Center, a Nevada-based family practice and urgent care facility. Barton had closed Kingsbury Urgent Care Center a decade earlier and wanted a presence in the state-line area once again. Negotiations soon led to the purchase of the Stateline Medical Center across the highway. Paul Marlowe, M.D., and Stephen Brooks, M.D., remained on board. The business was relocated almost directly across the street from the original site. Over the years, the medical and clinical support staff grew.
Just four years later, additional Barton outpatient services were added to the service mix in Nevada. Space was provided for oncology, urology, occupational health, rehabilitation (physical, occupational, and speech therapies), laboratory, medical imaging, mammography, and nutrition. Due to Barton’s strong rehabilitation program, Lake Tahoe Orthopedic Institute combined its Physical Therapy Department with Barton's department. By 2003, Tahoe Family Physicians (later Barton Family Practice) opened an office in the Nevada location as well. Urgent Care partnered with Family Practice to better serve their patients.
Although the facility is still known as Stateline Medical Center, the individual offices within the center were renamed Barton Urgent Care, Barton Family Practice, Barton Internal Medicine and Barton Pediatrics, Barton Laboratory, Barton Rehabilitation and Sports Medicine, and Barton Rheumatology to better reflect the connection to the Barton Health family.
On-Site Ski Clinics
With its experience operating the urgent care clinic at Kirkwood Mountain Resort, it was an easy decision for Barton to expand similar services to the other local ski areas. Barton Medical Clinic at Sierra-at-Tahoe was set up in a 34-foot mobile home until space was provided in the lodge in 2003. Barton Medical Clinic at Heavenly Mountain Resort was located in a modular unit at the bottom of the aerial tramway at the California Base Lodge. All clinics are staffed during the winter season with a physician, nurses, X-ray technicians, and nonclinical assistants. Clinics have expanded services and continue to see patients today during the ski season. Tahoe Emergency Physicians, Barton’s Emergency Department group, assisted with management of some of these facilities. The clinics have provided expeditious treatment and saved many patient trips to the emergency room.
Additional Acquisitions
As departments and support staff grew, so did the need for space. By 2006, off-site offices were purchased for home health, hospice, the hospital foundation, and public relations. A former doctor’s office located near the hospital was purchased and renovated for use by other physicians.
Barton Community Clinic
Clinic services also grew, both in 2004 and again in 2012, when construction began on a $1.4 million expansion, funded by the Barton Auxiliary and the Barton Foundation. The latest project will add a larger waiting room and more treatment rooms. Services continue to cover high-risk prenatal and gynecologic care and family planning, in addition to primary care.
The clinic treats an average of 1,600 patients each month, many of whom previously relied on the Emergency Department for their medical needs. It provides a medical home and treatment for those who can least afford it and also keeps costs of care lower for the entire patient population in the South Lake Tahoe region.
Lake Tahoe Surgery Center
Lake Tahoe Surgery Center, a partnership between BMJ Medical Management and 10 local physicians, opened in Roundhill in 1998. It was established by orthopedic surgeons who wanted an outpatient facility in Nevada. Its three ambulatory surgical suites gave residents an alternative to surgery at Barton. The surgery center impacted Barton’s surgical volumes, and BMJ eventually sold its shares; as a result Barton Health became a majority shareholder of the center in 2008. The two surgery options offer great choices for Barton’s community and physicians.
Executive Management
Tahoe Carson Valley Medical Group (TCVMG)
Numerous physician practices came under the Barton Health umbrella as the move for physician alignment continued across the country. Barton’s management philosophy encouraged collaboration and partnering. By 2012 TCVMG, which largely started as a family practice group, employed 25 physicians in eight multispecialty fields. This group then contracted physician services to Barton Health. The larger scale of participation allowed for better buying, negotiating, and contracting for services, with ultimate economic benefit for the patient. Physicians enjoyed the benefits of a patient practice without the additional challenges of running a business. More contracts are likely as physicians realize the benefits of this relationship.
Healing Design
The year 2003 began the shift to Healing Design at Barton. The Barton Foundation had laid the groundwork with a music and television system that offered soothing music and scenic visuals to reduce patient anxiety during hospitalization. Diane Bush, community member with professional experience in hospital redesign, contributed to the plan working with Vice President of Foundation and Public Relations Linda Thompson. Visitors appreciated the shift from white walls and mismatched furniture to calming themes; practical, comfortable seating; and original works of art. From the browns and oranges of the ’70s, the mauves and blues of the ’80s, and the “anything goes” clutter of the ’90s, colors and themes were thoughtfully chosen, with a focus on the patients’ peace of mind and recovery. The Lake Tahoe Art League partnered with the Barton Foundation to display the work of local artists on a rotating basis. The program gave the artists exposure, and sales of their work added contributions to the Foundation, which received a percentage of receipts. In 2006, the first patient room was remodeled with the healing design concept in mind. Within five years, all birthing suites and lobby areas were redecorated.
Nursing Program
To address the 2005 nursing shortage, Vice President of Hospital Operations Kathy Cocking found grant funding to create an online nursing program with Sierra College—the first such program in California. The California Board of Registered Nurses approved the program, and eight students enrolled and completed their degrees. The program continues today, with all hands-on rotations taking place in Sacramento hospitals. Four of the first graduates were employed at Barton Health immediately on graduation.
International Outreach
In 2005, after a tsunami and an earthquake hit Sri Lanka and India, Barton pitched in with a helping hand. The hospital sent thousands of dollars in supplies and cash to UC Davis Medical Center, where Sri Lanka native Tissa Kappagoda, M.D., collected much-needed resources for the 19 million people devastated by the catastrophe. Many Barton physicians continue to support medical programs internationally by traveling to foreign countries to contribute their services.
Guest Relations
In past years, guest relations educational seminars were periodically conducted at the hospital. In 2006, Barton made a commitment to the Disney Guest Relations program, later customized as the “Barton Way.” Ever since, patient satisfaction survey scores have risen dramatically. The commitment started at the top. Management and other leadership personnel attended a three-day intensive program at the Disney property. The theme of “Consistently Exceptional Care” was reinforced with the standards of safety, respect, image, and efficiency, and became part of the culture. Although the Barton Way is a recent innovation, the emphasis on guest relations is not new. Confirmation comes in the form of appreciative letters, in which patients acknowledge the employees and physicians who provide quality care, compassion, and professionalism. Hundreds of thank-you letters are received each year.
A Great Place to Work
During this decade, employee turnover at the hospital was half the national average, affirming that in both weak and strong economic times, Barton is a great place to work. Centralized hiring replaced scattered management practices. Hiring for cultural compatibility was factored into employee screenings. Personality assessments ensured an optimal fit between Barton and its employees.
Community Advisory Committee
In 2009, John G. Williams, CEO for Barton Health, identified the need for a Community Advisory Committee. With oversight from the hospital board of directors, a partnership was made up of representatives of public health agencies, school districts, physicians’ offices, nonprofit organizations, police, and other sectors. They agreed to meet each month to discuss health issues and identify areas of greatest need. With input from the committee, Barton Health has funded grants for community programs addressing health deficiencies since 2009.
Pulling Together
The recession left no one untouched. In response, Barton officials put a freeze on capital purchases, new hires, and conference expenditures. Prudent financial decisions included layoffs, early-retirement options, and reduced employee benefits. Barton's survival depended on a balanced budget. Cuts were made to the Employee Longevity program, which rewarded employees for their years of service. (That incentive was reinstated a year later when the outlook brightened.) Employer-matched retirement contributions were reduced. Employee insurance deductibles increased. In time, some laid-off personnel were brought back, while other responsibilities were absorbed by existing staff.
Unrest and difficult choices put a strain on the leadership team, which was eased by CEO John Williams’ calm demeanor and a cooperative spirit among the hospital team members. Enhanced employee communications practices and committee involvement helped facilitate the flow of information in both directions.
Disaster Preparedness
Barton Memorial Hospital began disaster planning soon after it opened in 1963, with yearly drills held to meet Joint Commission standards. Employees trained to be ready for all kinds of disasters, including casino fires, vehicle crashes, and boating collisions. September 11, 2001, made emergency management even more crucial. The Joint Commission doubled hospital requirements, mandating two annual disaster drills. In 2007, the Emergency Management Community Council (EMCC) was established, bringing emergency services together for better preparedness. Members included the hospital, South Lake Tahoe Airport and Police, the California Highway Patrol, local fire departments, CAL Star, El Dorado County Sheriff and Public Health, Search and Rescue, the American Red Cross, the Lake Tahoe Unified School District, the South Tahoe Public Utility District, Lake Tahoe Community College, ham radio operators, the U.S. Coast Guard, the U.S. Forest Service, and other partners. Barton took extra steps to safeguard its community. A trailer for chemical decontamination was purchased through a federal grant. A team was fitted for decontaminant suits and trained to deal with patients contaminated by chemical exposure. The team trained with the El Dorado County Hazardous Materials team and fire department hazmat teams.
Transitions in Care
With the greater need for disease management and to keep patients healthy at home instead of revisiting the hospital after a recent stay, Barton implemented the Transitions in Care program, based on a model created by Eric Coleman, M.D., and implemented by Mary Bittner, Vice President of Nursing for Barton Health.
The model employs nurses who visit patients in the hospital to review their post-hospital care. After the patients return home, the nurses stay in contact to discuss vital signs, physician's visits, diet, and other key indicators of health. The program has been successful in helping patients manage their illnesses and reducing return visits to the hospital.
Barton Health is Born
From a small community hospital, Barton has grown into a comprehensive consortium of medical services and providers. In 2010, while Barton Memorial Hospital retained its name, the larger system was renamed from Barton Health Care System to Barton Health to bring all the services and facilities under one medical management umbrella.
Helipad
The helipad was a hot topic in 1996 when the California Department of Transportation (Caltrans) made a site visit to the hospital and announced it was “nonconforming” with state standards. The close proximity of buildings and trees to the helicopter landing site was first identified as a matter of concern in 1980, when it was built. As word spread through the community, residents worried they may lose the lifesaving service, which had transported 87 patients in the first six months of 2000. A new location was sought, and three years later a new helipad was built directly above the Emergency Department on the canopy of the second floor, with all safety zones cleared of trees in accordance with state and federal standards. To enhance the appearance of the hospital grounds, many of the trees cut down to improve the flight path were carved into the shape of Sierra wildlife by local artist Jerry Toste.
Lake Tahoe: Still the Destination for Orthopedic Care
During the mid-2000s, Barton Orthopedists, led by Keith Swanson, M.D., introduced unicompartmental knee surgery, a procedure that allows physicians to replace only one side of the knee. This surgery has become more popular with active people opting for less than full knee replacement.
Robert Rupp, M.D., advanced Tahoe Orthopedics services when he started performing hip arthroscopies in the latter part of the decade.
With the economic turbulence that began in 2008, Barton Health and Lake Tahoe Surgery Center formed an alliance improving patient care. The outpatient surgery center provided a freestanding Nevada-based facility to offer patients more surgical choices utilizing the skills of the same physicians.
Tahoe Orthopedics and Sports Medicine became a Barton entity with physician partners Terrence Orr, M.D.; Stephen Bannar, M.D.; Daniel Robertson, M.D.; Robert Rupp, M.D.; Jonathan Finnoff, D.O.; and William Cottrell, M.D.; along with Kyle Swanson,M.D.; and Keith Swanson, M.D.
Barton Health solidified the concept of an orthopedic institute. Accreditation from Lake Tahoe Sports Medicine Fellowship raised awareness and acclaim for the Tahoe facility.
Lake Tahoe Sports Medicine Fellowship
The Lake Tahoe Medical Fellowship, established in 1984, reached a new benchmark in 2009. Thanks to the efforts of Dr. Clint Purvance, the orthopedic fellowship was accredited by the Accreditation Council for Graduate Medical Education. The new program, under the aegis of Barton Health, became known as the Lake Tahoe Sports Medicine Fellowship. The curriculum focused on orthopedic surgery with an emphasis on sports medicine and trauma. Fellows rotated through surgical and clinical settings, working side by side with board certified orthopedic surgeons.
Fellows applied for training after completing medical school and residencies. The one-year fellowship program set the stage for hands-on training with prequalified orthopedic physicians to train, teach, and expose Fellows to real-patient situations, including the most challenging cases. Since the accreditation, competition to enroll in the program has increased, and more and more postgraduate orthopedic surgeons, hoping to come to Tahoe to live and learn, vie for the two annual openings. To date, more than 100 students have completed the sports medicine fellowship in Lake Tahoe.
Although practicing orthopedic physicians educate the Fellows, it also became common for these Fellows to bring the latest techniques from their residencies to Lake Tahoe. Military medical officers who joined the program brought unique experience with trauma, from which local physicians could learn.
Lake Tahoe’s orthopedic surgeons maintained an outstanding reputation. At times, up to 70 percent of our orthopedic patients came from out of the area, a testament to the caliber of Barton physicians.
Together, the practices of Tahoe Fracture Clinic (TFC) and Tahoe Orthopedics and Sports Medicine (TOSM) provided a full scale of orthopedic care. While TOSM is managed by Barton Health, TFC remained an independent physician practice. Carrying orthopedic care to a new level, the Tahoe Center for Orthopedics (TCO) evolved, which embraces the orthopedic practices in a patient-centered model that includes all aspects of care including rehabilitation, home health, medical imaging, nursing, education, surgery, and more.
The TCO developed into a nationally recognized, comprehensive, patient-centered orthopedic program focusing on quality and personalized care, covering the full spectrum of musculoskeletal injury and disease. A nurse navigator ensured every step was managed efficiently and effectively for the best possible outcomes.
The TCO also partnered with local schools, scheduling presentations, outreach, screenings, athletic training and vocational opportunities. The future affords opportunity for high-altitude training programs and partnerships with Olympic athletes. Terrence Orr, M.D., has served as the head physician for the Men’s U.S. Alpine Ski Team with four additional staff members, Stephen Bannar, M.D., Kyle Swanson, M.D., Jonathan Finnoff, M.D., and Daniel Robertson, M.D., serving on the U.S. Ski and Snowboard medical team. Tahoe Center for Orthopedics is a natural next step in the development of a destination orthopedic center.
When Disaster Struck, The June 2007 Angora Fire
For decades, disaster drills were conducted countywide to help community agencies prepare in case of emergency. Many residents acted as patients in mock disaster drills, which gave the community a better understanding of who would respond to a large-scale disaster and how the agencies would interact.
On June 21, 2007, the management of Barton HealthCare System participated in a mandatory emergency-preparedness training session. Darcie Carpenter, emergency management coordinator, reviewed basic training and real-life scenarios, and ended with tabletop drills.
Just three days later, on June 24, the timing of those drills seemed prophetic with the onset of one of the region’s worst disasters.
Swift Response
The historic Angora Fire started in the heavily forested region west of North Upper Truckee Road below Echo Summit. The first 911 call was recorded at 2:10 p.m. By 4 p.m., Barton had established an incident command center, managed by Vice President of Hospital Operations Kathy Cocking.
Due to high winds and other factors, the fire spread rapidly. Carpenter was relocated to the emergency operations center with other emergency responders. At the command center, the hospital management team assessed the situation, maintained communications with frontline emergency crews, and surveyed the available resources. Clinical staff and physicians evaluated patient safety, bed availability, and staffing. Leaders shared information about supplies, patient transport options, security, and communications.
Growing Threat
Barton was located just one mile from the wall of flames, which had climbed 60 feet high. Because the hospital might be forced to evacuate, emergency patients were swiftly transported to Carson Tahoe Hospital or Renown Health. Nonemergency patients were encouraged to travel across town to Stateline Medical Center to free up the Emergency Department for potential fire victims. As the fire continued to rage, all ambulatory surgeries were canceled and outpatient services were diverted to off-site facilities.
The skies filled with smoke and the air quality deteriorated. Health issues were a concern, so officials evacuated 39 elderly residents of Barton’s Skilled Nursing Facility (SNF). In orderly, “field trip” style, the residents were escorted safely onto BlueGo buses and transported to Carson Valley Residential Care Center, more than an hour away.
SNF staff accompanied the patients and stayed with them for the entire three-day excursion. It proved a fun outing for the residents, who were unaware of the danger.
The Aftermath
The incident command center would not close until the fire was 80 percent contained—five days after it started. When the firestorm was finally over, 3,100 acres had been destroyed along with 254 homes, 67 commercial buildings, and 35 other structures. Though 2,174 firefighting agencies responded at a total cost of $12.1 million, all that remained of the homes were charred foundation slabs, ashes, metal vehicle frames, and memories. Several firefighters were injured, but thankfully, no lives were lost.
The Barton employee family later determined that 147 employees had been evacuated from their homes and 16 employee/physician houses had burned to the ground.
Support was strong in the community, which was quick to help those in need. Counseling sessions were provided for all Barton staff members. Friends and strangers alike opened their homes, hearts, and pocketbooks to help.
Rebuilding the Emergency Plan
When disaster strikes, responders can push themselves beyond reasonable limits, leading to anxiety and exhaustion. In the aftermath of the Angora Fire disaster, Barton Memorial Hospital boosted its emergency-preparedness plan in case of future disasters. The plan included training backup support to help personnel at the incident command center; strengthening relationships with community partners; and compiling and maintaining contact data for all agencies. The nuts-and-bolts plan was detailed down to the stockpiling of backup radio batteries, cellphone chargers, and other important supplies.
2010s - EXPANDING SERVICES AND CARE

American healthcare experienced a large transformation with the passage of the Affordable Care Act in 2010. With a goal to increase health insurance coverage to more Americans and a focus on preventative medicine, the Affordable Care Act led to a decade of changes for health systems across the county.
Barton Health’s transformation ensured our patients are able to organize their health digitally through an electronic medical record system, partner with their primary care team to proactively manage their health, and receive annual wellness checks and preventative screenings each year.
Patient Care
daVinci Surgical System
In 2012, Barton Memorial Hospital welcomed a new addition to its surgical team – the da Vinci® Si Surgical System. One of the first hospitals in the area to make this technological investment, the da Vinci Si is an effective alternative to both traditional "open" surgery and conventional minimally invasive laparoscopy and the benefits to patients include a shortened hospital stay, reduced infection risk, and less blood loss, pain, and scarring.
In 2019, Barton again embraced the latest in surgical technology with the acquisition of the updated da Vinci Xi Surgical System. Key features include a new overhead instrument arm to replicate the surgeon’s anatomical access, improved vision definition and clarity, and a greater range of motion.
Cardiology
Continuing its growth of medical services and recruitment of specialized physicians to Lake Tahoe, Barton Cardiology launched in 2012, with the arrival of Lake Tahoe’s only full-time cardiologist, Dr. David Young.
MyChart
With the launch of MyChart in 2014, Barton Health’s patients now had the ability to access their health care in the palm of their hand — and around the clock. Connected to EPIC, Barton electronic medical record system, MyChart is a website and app that provides patients a convenient and secure way to view their medical information and stay in touch with their health care providers.
Urology
In 2014, Barton Urology opened to meet patient needs for specialty care close to home. Barton Urology is available to treat a full-range of urologic conditions in men and women of all ages, in addition to robotic urological surgical procedures.
Level III Trauma Center
In 2015, Barton Memorial Hospital was designated a Level III trauma center making it, at the time, the only trauma center in the Lake Tahoe, Truckee, and Carson Valley region. Verified Level III trauma centers must meet, at a minimum, more than 160 different essential criteria and guarantee the resources for trauma care and the immediate availability of emergency medicine physicians, surgeons, nurses, lab and x-ray technicians, and life support equipment 24-hours a day.
As a designated trauma center, Barton is prepared to treat severe injuries, while also working to keep people out of the Emergency Department through community outreach and injury prevention programs.
Palliative Care
Identifying a need for a comprehensive support system for patients with serious or terminal illness, Barton Palliative Care, now Barton Advanced Care, opened in 2016. Palliative care is available at any stage of a serious or terminal illness — not limited to end of life or Hospice care. Patients facing serious illness may live for years and a palliative care plan helps relieve patient’s pain, symptoms, and stress levels.
Barton Performance
In 2016, Barton Performance launched its innovative service, focusing on helping community members of all abilities eat well, train well and restore well for whole-body health, optimal performance and injury-reduction. Different from a gym or health club, Barton Performance integrates medical involvement with Barton Health’s high-level orthopedics and rehabilitation programs as needed, to help patients get back to enjoying their Lake Tahoe lifestyle.
In 2018, Barton Performance moved from its facility on Emerald Bay Road into the state-of-the-art Robert Maloff Center, providing physical proximity to sports medicine practitioners and industry-leading training equipment.
Maternal Safety
In 2017, Barton Memorial Hospital had one of the lowest C-section rates of birthing hospitals in the state, according to the California Health and Human Services Agency. And reinforcing Barton Health’s commitment to quality maternal care, Barton Memorial Hospital was designated a Blue Distinction® Center for Maternity Care, a result of its expertise in delivering improved patient safety and better health outcomes.
Best Clinical Application
The Joint Commission recognized Barton Memorial Hospital’s capnography program for “Best Clinical Application” in 2017. A capnography machine is a respiratory device that monitors a patient’s breathing during anesthesia and intensive care. By reviewing and improving prevention processes and implementing awareness programs in the last four years, Barton Hospital greatly reduced risks and improved patient safety. This included reduction of patient narcotic usage, improved identification methods for at-risk patients, and additional physician and staff education.
Barton Center for Orthopedics & Wellness
Launched in 2018 and transformative in nature, the Barton Center for Orthopedics & Wellness was designed to improve the health of the community by combining traditional orthopedic medical care with personalized rehabilitation and sports performance and integrative medicine and wellness treatments such as nutrition counseling, health coaching, and acupuncture. This proactive approach not only gets the patient moving again, but back to their active lifestyle – whether competing in Olympic trials or day hiking with grandchildren.
The 26,000 square foot state-of-the-art medical facility houses the latest in rehabilitation and sports performance equipment, giving patients and local athletes access to a world-class facility while receiving expert support to achieve their goals.
Outside the Robert Maloff Center, a trail network leads into Johnson Meadow, adjacent to the facility. As part of its commitment to community health and helping residents and visitors enjoy the great outdoors, Barton contributed $50,000 to the acquisition of Johnson Meadow – 206 acres of the Upper Truckee watershed east of the Center — to ensure access to trails and connect patients with the role nature plays in personal well-being.
Barton Neurology
Launched in 2019, Barton Neurology expanded Barton’s patients’ access to care and treatment of neurological issues including disorders of the nervous system, such as Multiple Sclerosis, Parkinson’s disease, epilepsy, stroke, vertigo and memory conditions such as Alzheimer’s Dementia. In addition to these conditions, Barton Neurology is able to treat concussions and spinal cord issues, integrating with the health system’s well-known orthopedic services.
MAT Program
In an effort to address the opioid crisis and help community members struggling with substance abuse, Barton Community Health Center (BCHC) launched a Medication-assisted Treatment (MAT) Program. Practitioners with BCHC treat patients presenting withdrawal symptoms in Barton’s Emergency Department, or with a doctor’s referral at Barton Community Health Center, using both medication and specialized therapy to help patients manage and quit narcotic dependence.
Sports Medicine Specialists
Concussion Management
In an effort to reduce complications associated with concussions and promote concussion injury awareness in student athletes, Barton launched concussion testing at area high schools including South Lake Tahoe, Whittell, and Douglas High in 2011. Concussion testing is among one of the many medical services provided by Barton Health’s athletic trainers. Athletic Trainers also treat a variety of sports medicine injuries on the sidelines and in the training room.
Olympic Care
In 2014, Terrence Orr, MD, and Jonathan Finnoff, DO, both physicians with Tahoe Orthopedics and Sports Medicine, volunteered as team physicians at the Winter Olympics in Sochi, Russia. Remaining healthy is one of the keys to an Olympic athlete’s success, and while sports-related injuries are certainly part of what Dr. Orr and Dr. Finnoff treated, medical concerns for athletes covered a broad range of medical issues, including infections and asthma.
US Ski and Snowboard Association Award
After nearly 30 seasons, the U.S. Ski and Snowboard Association (USSA) recognized Dr. Terry Orr of South Lake Tahoe as the 2016 recipient of the John J. Clair Jr. Award given annually to a person who provides exceptional service to the U.S. Ski Team or U.S. Snowboarding. Dr. Orr volunteered for U.S. Ski and Snowboard since 1988 and served as the Head Team Physician for USSA Men’s Alpine for 14 seasons. He helped create and develop the USSA Medical Pool and Medical Committee and volunteered to provide medical coverage for numerous athletic events, including four Winter Olympics.
Leading Spine & Back Care
In 2017, Barton Health welcomed South Lake Tahoe native, Dr. Zachary Child, as a member of the renowned orthopedic team. Skilled in addressing back pain and finding surgical and non-surgical options that help patients reach optimal spine health, Dr. Child is a board-certified orthopedic spine surgeon and musculoskeletal oncologist.
Facilities Management
Barton Community Health Center
In 2013, the Barton Community Health Center was expanded to accommodate more patients and increasing operational needs. Growing to more than 7,000 square-feet and 18 patient rooms, the larger facility can offer increased services including physical examinations, diagnosis and treatment of acute health problems, orders, lab work and X-rays, well-child care check-ups, specialty care and other necessary treatments.
Funding for the expansion came from the Barton Memorial Hospital Auxiliary who raised nearly $800,000 and the Barton Foundation which generated nearly $140,000 from their fundraising efforts through the annual Festival of Trees and Lights and other donor opportunities.
Barton Goes Smoke Free
Always dedicated to improving the health of our patients, employees, and our community, Barton Health adopted a healthcare system-wide, smoke-free policy in 2014, joining hospitals across the nation to promote a healthy environment.
Robert Maloff Center
In the history of philanthropy, there are names that shine brightly, leaving a lasting impact on the communities they touch. Robert and Lisa Maloff represent one story, whose commitment to giving back helped shape the South Lake Tahoe community. At Barton, the Robert Maloff Center, home of the Barton Center for Orthopedics & Wellness, serves as a testament to their caring and generosity.
In 2015, Lisa pledged $10 million toward the construction of the Robert Maloff Center, a state-of-the-art facility adjacent to Barton Health’s hospital campus, with the goal of bringing together a focus on wellness, sports performance, orthopedics, and rehabilitation — a therapy pool inside the Robert Maloff Center was funded by a $1 million donation from the family of Dr. Paul Fry II, the Maloff’s close friend and a renowned orthopedic surgeon.
Executive Management
Barton Welcomes a New CEO
After nine years, Barton Health CEO John G. Williams passed the baton to Barton’s Chief Medical Officer, Dr. Clint Purvance. Dr. Purvance has practiced at Barton Memorial Hospital as an emergency room physician since 1999 and was Chief Medical Officer since 2007.
“Mr. Williams has done a remarkable job leading Barton Health,” says Kirk Ledbetter, chairman of Barton Health’s Board of Directors. “He has led the organization into a position of solid financial health and has built a strong team of leaders to face future challenges.”
And in a statement released to physicians and staff, Kirk Ledbetter expressed his and the Board of Directors excitement about the future of Barton Health, “the Board of Directors is confident that Barton Health’s patients, employees, physicians, and community are in good hands,” said Ledbetter. “Dr. Purvance has the skills, knowledge, and leadership to guide us through Barton Health’s next chapter of health and wellness in our community.”
Community Outreach
Enrollment Counseling
Signing up for health insurance can be a frustrating and time-consuming process. To ease the insurance buying process, Barton Health partnered with Covered California, California’s Insurance Exchange Marketplace, to assist community members when signing up for health insurance through the exchange marketplace. Though Covered California does not reimburse Barton for the Enrollment Counselors, it was important to donate staff time to support our community during the monumental Affordable Care Act transition.
Mental Health Action Plan
In 2015, more than 80 individuals made an action plan at the collaborative Mental Health Forum to address the gaps with mental health services in the South Lake Tahoe community. At the forum, medical providers, law enforcement, social service groups, school district staff, and community members discussed professional and personal experiences with every age level, and offered their insights and ideas. Sub-groups then transformed the insights and ideas into action items and next steps to improve the community’s state of mental health.
Strategic Partnerships
Gene Upshaw Memorial Tahoe Forest Cancer Center
Barton Health has partnered with the Gene Upshaw Memorial Tahoe Forest Cancer Center, a service of Tahoe Forest Health System, located in Truckee, CA in 2013 to expand its oncology services for cancer patients who reside in the South Lake Tahoe area. For cancer patients, who are in-between chemo doses, the program not only minimizes stress and travel expenses, but also saves patients time where they need it most – to heal.
American Council of Graduate Medical Education
In 2016, the American Council of Graduate Medical Education (ACGME) identified Barton Health, in conjunction with its Lake Tahoe Sports Medicine Fellowship program, as an accredited Graduate Medical Education institution. In addition to its highly-competitive sports medicine fellowship, general surgery and urology residents from the University of California, Davis School of Medicine and medical students from the University of Nevada School of Medicine conduct clinical rounds in the hospital and outpatient clinics as part of their clinical training in partnership with Barton Health.
UC Davis Cancer Care Network
Barton Oncology proudly partnered with UC Davis Health to provide cutting-edge care in the fight against cancer. As part of the UC Davis Cancer Care Network, patients at Barton Health have access to advanced cancer care provided by leading academic specialists at the National Cancer Institute-designated UC Davis Comprehensive Cancer Center with the consistently exceptional care they have come to know and expect at Barton Health.
U.S. Forest Service
Solidifying a nationally recognized community wellness program, Barton Health and the Lake Tahoe Basin Management Unit (LTBMU) signed an agreement in 2017 for cooperative Wellness Outings: guided walks that promote nature as medicine by teaming patients with a U.S. Forest Service ranger and physicians or nurses from Barton Health for guided outings in the national forest. In addition to Wellness Outings, the partnership will provide wellness and injury prevention trainings for USFS rangers and firefighters, as well as accessibility of public lands to promote outdoor recreation.
Auxiliary
Funding Technological Advancements
In addition to the Barton Community Health Center expansion project, the Barton Auxiliary donated $220,000 in 2015 to purchase the latest in medical imaging technology, a 3D tomosynthesis mammogram machine, ushering in a new era in local cancer screenings and community health in Lake Tahoe.
Dan Kerr’s Lasting Legacy
Barton Health Auxiliary member, Dan Kerr had coordinated the Barton Auxiliary Blood Drive held every other month, donated more than 26 gallons of blood since 1981, and served as Auxiliary President for six terms, and when he passed away in 2014, he left a lasting legacy with his donation of $219,097.92, divided equally, to the Barton Auxiliary and Barton Foundation. The Barton Auxiliary pays his philanthropic efforts forward to local students pursuing careers in healthcare through the annual Dan Kerr Scholarship.
Dream Chaser: A Barton Patient's Heroic Fight to Run Again
It was August 2013 when Kyle Van Mouwerik was recovering from a bout of strep throat but the pesky low grade fever and body fatigue lingered. Chalking them up to residual strep symptoms, the extremely fit 22-year-old returned to work as a wildland firefighter with the Tahoe Douglas Fire Protection District in Lake Tahoe, NV. Shortly after returning, the crew was called to a fire in Elko, NV. It was there that Kyle started feeling the weakness and tingling in his feet. Unable to walk, he was taken to Emergency Department at Northeastern Nevada Regional Hospital where he went from battling a wildland blaze just hours before to battling for his own survival.
Within two hours of his arrival at the ED, Kyle was diagnosed with Guillain-Barré syndrome (GBS), a disorder in which the body's immune system mistakenly attacks the nervous system. While not contagious, the syndrome is rare, afflicting only about one person in 100,000. In the following hours, Kyle was airlifted to Reno and over the next four days, GBS began attacking his respiratory functions making it impossible for him to breathe. He was put on life support and spent the next month in a drug-induced coma. When he awoke, Kyle was paralyzed from the neck down; only able to move his head side to side and make slight movements on the right side of his face.
The healthy young man who had aspirations of becoming a paramedic firefighter found himself confined to a wheelchair, unable to feed himself, and facing a long recovery. Over the next two years, Kyle embarked on a courageous and inspirational journey of self-discovery and healing.
Typically during the onset of GBS, hands and feet are the first extremities affected but in recovery they are the last to regain feeling and strength. Patiently and painfully undergoing weekly rehabilitation sessions Kyle had to wear heavy, cumbersome support braces to keep his body weight from fracturing his bones due to severe muscle atrophy. But he gradually progressed from walking for a few pain-filled minutes each day to walking for a few hours each day.
By February 2015, Kyle was walking on his own, but still unable to run. He was looking for other rehabilitation options when he heard about the AlterG anti-gravity treadmill at Barton Health. Designed to help patients run and walk without having to bear their full body weight, the treadmill reduces exercise impacts and lessens joint compression to optimize rehabilitation and physical therapy outcomes. Its differential air pressure technology allows precise unweighting, up to 80 percent of a person’s body weight.
After nearly two years of rehabilitation Kyle ran on the AlterG for the first time. “I almost started crying,” he said. “It was such a spiritual experience. I don’t see it as just a workout; it’s just beautiful.”
Alan Barichievich, Barton Health’s Rehabilitation & Sports Medicine director was with Kyle the day he ran for the first time on the AlterG. “In the 20 years of being in the rehabilitation business, this was one of the coolest moments I have ever experienced,” says Alan. “He was the happiest person in the world and I just felt so lucky to be a part of his joy.”
The two worked closely to create specially-designed orthotics to help Kyle with his running gait and create additional support required for him to continue training. Today, Kyle is running twice a week for 30 minutes on the treadmill. “Being able to work out on the AlterG provides me with the opportunity to step my workout up slowly so I can achieve my goals in a healthy fashion,” he said.
Kyle has never lost sight of his goals. This March, the well-spoken 24-year-old enrolled in paramedic school. He hopes to finish his schooling by year’s end and achieve his dream of becoming a paramedic firefighter. Kyle also has been named the Reno region’s liaison for GBS Foundation International, a foundation created to provide GBS suffers with a support network. “I experienced something in my life that most people never will. Now I feel a responsibly to make it better for people who go through an experience like mine.”
2020-2023 - OVERCOMING CHALLENGES

The early years of the 2020s brought new challenges to Barton Health, Lake Tahoe, and the world with the COVID-19 (coronavirus) pandemic and 221,835 acre Caldor Fire dominating Barton’s operational focus for much of 2020 and 2021.
COVID-19
The COVID-19 pandemic forced the world to rapidly adapt and Barton was no exception. As the virus swept the globe, a coordinated internal response and collaboration with regional medical organizations and government agencies allowed Barton to continue to provide vital care to the community, maintain essential services, and manage resources efficiently.
Barton Health, in partnership with the Centers for Disease Control & Prevention (CDC) and California Department of Public Health (CDPH), began preparing for the spread of coronavirus (COVID-19) since the emergence of the outbreak in late 2019. By March 2020, Barton had launched its Hospital Incident Command System (HICS) to comprehensively coordinate and organize teams to care for a possible surge of patients.
To help protect the community, Barton launched a 24/7 COVID-19 health line for patients to receive virtual COVID-19 screening and guidance, and alternative care and testing sites were launched, ensuring patients and health care providers’ safety, while also keeping the Emergency Department open for emergent care needs. In-office medical care was shifted to virtual visits whenever appropriate, helping to reduce the risk presented from shared reception areas and patient congregation.
Within the hospital, where patients needed critical care, Barton transformed 68 patient rooms into negative pressure environments, lowering the risk of airborne spread. A new partnership with Eagle Telemedicine was developed to assist the treatment of patients admitted to our Intensive Care Unit related to their COVID-19 diagnosis, reducing the need to transfer critically ill patients.
To help offset the financial burden related to the COVID-19 lockdown, the Barton Health Foundation launched the COVID-19 Response Fund, initially matching donations up to $75,000 for impacted community members. The COVID-19 Response Fund also organized efforts related to obtaining and distributing Personal Protective Equipment (PPE) and face masks to help protect frontline workers throughout the pandemic.
In December 2020, newly developed vaccines became available and by spring 2021, Barton vaccinated more than 5,000 people including employees and community members.
By the end of the pandemic in May 2023, Barton had spent over $4 million on facility updates, supplies and Personal Protective Equipment (PPE) and developed COVID-19-related programs including rehabilitation services for patients experiencing lasting effects from their COVID-19 illness. Many of the programs quickly adopted in the height of the pandemic, like virtual visits and specialized telemedicine partnerships, continue to improve patient care and provider access for our community.
Caldor Fire
The Caldor Fire swept through our region during summer 2021, presenting another formidable challenge: safely evacuating the entire hospital of all patients and residents, then ceasing all operations as the entire city of South Lake Tahoe was ordered to evacuate.
As the fire burned just over the summit, Barton opened its Hospital Incident Command System (HICS) to coordinate safety efforts related to smoke mitigation and prepare for the possibility of fire within the Lake Tahoe basin.
When the fire approached Echo Summit, in coordination with Cal Fire’s Incident Management Team and California Department of Public Health, Barton Memorial Hospital was evacuated and closed; its Emergency Department team was the last clinical team to leave the hospital, staying open as long as possible.
Simultaneously, other Barton teams were opening a triage clinic at the fire operations’ base camp to help meet the medical needs of the thousands of fire personnel fighting the fire in our own backyard.
The Caldor Fire crested Echo Summit, miraculously spared Christmas Valley, continued to burn in the forests surrounding South Lake Tahoe, but was eventually contained and suppressed without burning any homes within the Tahoe basin.
With the repopulation of the city of South Lake Tahoe, Stateline and Zephyr Cove communities, Barton Memorial Hospital reopened and again delivered health services to its patients and Skilled Nursing Facility residents.
Throughout the Caldor Fire emergency, the Barton Health Foundation worked to meet community needs, and in less than a month more than $133,000 was raised and immediately distributed to assist residents and area food banks through the Caldor Response Fund.
Patient Care
UC Davis Health Partner
Barton expanded its relationship with UC Davis Children’s Hospital in Sacramento to increase Barton’s ability to care for more at-risk newborns by providing access to UC Davis specialists and experts including a neonatologist, and neonatal specialists within the pharmacy, respiratory therapy and nutrition departments. Additionally, Barton team members can access education opportunities through UC Davis Health to ensure training and new skill acquisition.
Plastic & Reconstructive Surgery Services
Barton welcomed Dr. Kathleen Holoyda, a plastic and reconstructive surgery specialist to lead Barton Plastic & Reconstructive Surgery, a new service offering solutions for patients who seek to improve form and function through reconstructive surgery, or improve appearance through aesthetic surgery, both of which can boost self esteem.
OB/GYN Expands to the Carson Valley
Barton Obstetrics & Gynecology (OB/GYN), formerly Barton Women’s Health, opened a new, second location in Minden, Nevada to better serve the growing Carson Valley and its resident’s health needs.
Certified Nurse Midwives Join the Care Team
Two certified nurse midwives joined Barton Obstetrics & Gynecology (OB/GYN), providing comprehensive care for low-risk, healthy pregnancies. Certified nurse midwives are often present during labor and delivery, offering experienced, compassionate support during birth and once the child arrives, in addition to performing pelvic and wellness exams, diagnosing gynecological challenges like yeast infections or sexually transmitted diseases, and treating common concerns such as urinary tract infections.
Orthopedics, Sports Medicine, and Rehabilitation Technology Shines
Ensuring the highest quality medical care for patients, Barton invested in the latest joint replacement technology that will enhance the patient experience for total knee, total hip, and partial knee replacements: Mako SmartRobotics.TM With Mako SmartRobotics, the robotic system enables orthopedic surgeons to have a more predictable surgical experience with increased precision and accuracy, resulting in better outcomes for patients.
Barton Rehabilitation Services invested in new technology to help patients relearn to walk and achieve mobility goals; the Bioness Vector Elite Gait and Safety System is designed to improve treatment efficiency, reduce patient falls, and prevent clinician injuries. Utilizing the system, Barton Rehabilitation will continue to rehabilitate patients recovering from stroke and amputations, orthopedic, brain and spinal cord injuries, and other neuro-cognitive disabilities return to daily activities in a safe manner.
Barton Health Foundation
Heart Safe Community
The Heart Safe Community program, sponsored by the Barton Health Foundation, is a community-wide effort aimed at educating citizens on the dangers of Sudden Cardiac Arrest (SCA). The Heart Safe Community program is based on strategic placement of and easy access to automated external defibrillators (AEDs) in public gathering spots throughout the South shore of Lake Tahoe.
Regional Expansion Project
Furthering its mission of improving community health and well-being, the Barton Health Regional Expansion Project will broaden regional medical services and allow for continued delivery of high-quality health care across the South Shore.
California 2030 Seismic Regulations
Barton Memorial Hospital will no longer meet California’s seismic safety regulations scheduled to take effect by 2030; therefore, the hospital must be rebuilt.
Rebuilding and retrofitting the current hospital facility would require a complex and financially-prohibitive staging and moving of patient care services while the project is constructed in multiple, years-long phases.
With a physical proximity to Nevada, fiscal responsibility demanded assessment of both California and Nevada locations to understand cost, timelines, patient care disruption, and growth opportunities in each location to best meet the needs of the future.
Planning for a Nevada-based Hospital
Guided by input from community surveys, stakeholders, partner agencies, and physician and staff teams, along with data from the triennial Community Health Needs Assessment (CHNA), market trends, current health data, state regulations, and CA 2030 seismic requirements for healthcare facilities, project planning for a newly constructed hospital in Stateline, Nevada is underway.
A new hospital will adjust to the future needs of healthcare — and the move six miles east will affect a very small percentage of patients, as the most frequently used services within the health system will not be affected by the relocation of the hospital facility. Barton is committed to the South Shore community and will continue to have robust outpatient services at the California campus in South Lake Tahoe.