Barton is one of the first hospitals in the Lake Tahoe and Carson City areas to offer Mako SmartRobotics™, a robotic system that enables orthopedic surgeons to have a more predictable knee and hip joint replacement surgical experience with increased precision and accuracy, resulting in better outcomes for patients.
In clinical studies, Mako Total Knee demonstrated the potential for patients to experience less pain, less need for pain relievers, less need for inpatient physical therapy, reduction in length of hospital stay, improved knee flexion, and soft tissue protection in comparison to manual techniques.
Scan. Plan. Mako Can.
We understand that knowing what to expect from your joint replacement experience is important to you. As you are reading through this material, please reach out to us to discuss if you have additional questions.
 Each patient is unique and can experience joint pain for different reasons. It's important to talk to us about the reason for your joint pain so you can understand the treatment options available to you. Pain from arthritis and joint degeneration can be constant or come and go, occur with movement or after a period of rest, or be located in one spot or many parts of the body. It is common for patients to try medication and other conservative treatments to treat their knee or hip pain. If you haven't experienced adequate relief with those treatment options, you may be a candidate for Mako Total Knee, Total Hip, or Partial Knee replacement.
Each patient is unique and can experience joint pain for different reasons. It's important to talk to us about the reason for your joint pain so you can understand the treatment options available to you. Pain from arthritis and joint degeneration can be constant or come and go, occur with movement or after a period of rest, or be located in one spot or many parts of the body. It is common for patients to try medication and other conservative treatments to treat their knee or hip pain. If you haven't experienced adequate relief with those treatment options, you may be a candidate for Mako Total Knee, Total Hip, or Partial Knee replacement.
Mako can help us plan for better outcomes, like less pain and shorter recovery times, compared to manual joint replacement surgery.1,2,3
How Mako works
Mako is an innovative solution for many suffering from painful arthritis of the knee or hip.
Scan. It all starts with a CT scan so your surgeon can know more about your anatomy.
Plan. The CT scan is used to create a 3D CT-based model of your joint. Your surgeon uses this 3D model to create a personalized surgical plan and assist your surgeon in performing your joint replacement procedure.
Mako Can. In the operating room, your surgeon follows your personalized surgical plan while preparing the bone for the implant. The surgeon guides Mako’s robotic arm within the predefined area, and Mako’s AccuStopTM technology helps the surgeon stay within the planned boundaries that were defined when the personalized preoperative plan was created.
It’s important to understand that the surgery is performed by an orthopaedic surgeon, who guides Mako’s robotic arm during the surgery to position the implant in the knee and hip joints. Mako does not perform surgery, make decisions on its own or move without the surgeon guiding it. Mako also allows your surgeon to make adjustments to your plan during surgery as needed.
Total knee vs. partial knee replacement
Based on the severity of the arthritis in the knee, total or partial knee replacement may be recommended by a surgeon. Both procedures involve the orthopaedic surgeon guiding Mako’s robotic arm to remove diseased bone and cartilage.

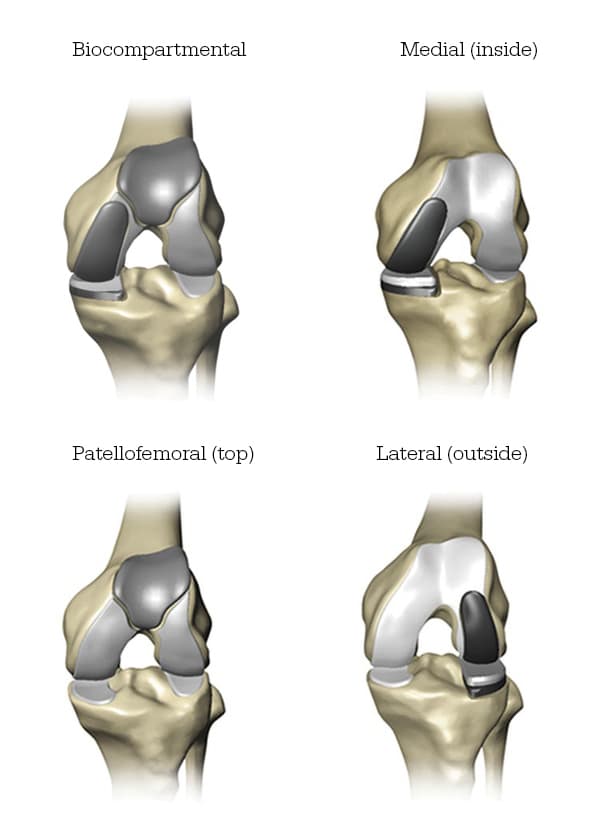
- Mako for Partial Knee replacement is a treatment option for adults living with early- to midstage osteoarthritis (OA) that has not yet progressed to all three compartments of the knee. Depending on where the arthritis affects the knee, patients may have an implant inserted in any of the following areas:
- In comparison, Mako for Total Knee replacement is a treatment option for adults living with mid- to late-stage osteoarthritis of the knee. With a Mako Total Knee replacement, the entire knee joint is replaced, and the surgeon inserts a Triathlon Total Knee implant. With over a decade of clinical history, Triathlon knee replacements are different than traditional knee replacements because they are designed to work with the body to promote natural-like circular motion.4-6
- Mako for Total Hip replacement is intended for patients who suffer from noninflammatory or inflammatory degenerative joint disease (DJD). Some forms of DJD include osteoarthritis (OA), post-traumatic arthritis, rheumatoid arthritis (RA), avascular necrosis (AVN) and hip dysplasia.
IMPORTANT INFORMATION
Knee & hip replacements
Knee and hip replacement is intended for use in individuals with joint disease resulting from degenerative and rheumatoid arthritis, avascular necrosis, fracture of the neck of the femur or functional deformity of the hip.
Knee joint replacement is intended for use in individuals with joint disease resulting from degenerative, rheumatoid and post- traumatic arthritis, and for moderate deformity of the knee.
Joint replacement surgery is not appropriate for patients with certain types of infections, any mental or neuromuscular disorder which would create an unacceptable risk of prosthesis instability, prosthesis fixation failure or complications in postoperative care, compromised bone stock, skeletal immaturity, severe instability of the joint, or excessive body weight.
Like any surgery, joint replacement surgery has serious risks which include, but are not limited to, pain, infection, bone fracture, change in the treated leg length (hip), joint stiffness, hip joint fusion, amputation, peripheral neuropathies (nerve damage), circulatory compromise (including deep vein thrombosis (blood clots in the legs)), genitourinary disorders (including kidney failure), gastrointestinal disorders (including paralytic ileus (loss of intestinal digestive movement)), vascular disorders (including thrombus (blood clots), blood loss, or changes in blood pressure or heart rhythm), bronchopulmonary disorders (including emboli, stroke or pneumonia), heart attack, and death.
Implant related risks which may lead to a revision of the implant include dislocation, loosening, fracture, nerve damage, heterotopic bone formation (abnormal bone growth in tissue), wear of the implant, metal and/or foreign body sensitivity, soft tissue imbalance, osteolysis (localized progressive bone loss), audible sounds during motion, reaction to particle debris , and reaction to metal ions (ALTR). Knee and hip implants may not provide the same feel or performance characteristics experienced with a normal healthy joint.
The information presented is for educational purposes only. Speak to your doctor to decide if joint replacement surgery is appropriate for you. Individual results vary and not all patients will return to the same activity level. The lifetime of any joint replacement is limited and depends on several factors like patient weight and activity level. Your doctor will counsel you about strategies to potentially prolong the lifetime of the device, including avoiding high-impact activities, such as running, as well as maintaining a healthy weight. It is important to closely follow your doctor’s instructions regarding post-surgery activity, treatment and follow-up care. Ask your doctor if a joint replacement is right for you.
Stryker Corporation or its other divisions or other corporate affiliated entities own, use or have applied for the following trademarks or service marks: AccuStop, Mako, Stryker, Triathlon. All other trademarks are trademarks of their respective owners
References
- Kayani B, Konan S, Tahmassebi J, Rowan F, Haddad F. An assessment of early functional rehabilitation and hospital discharge in conventional versus robotic-arm assisted unicompartmental knee arthroplasty: A PROSPECTIVE COHORT STUDY Bone Joint J 2019;101-B:24–33
- B. Kayani, S. Konan, J. Tahmassebi, J. R. T. Pietrzak, F. S. Haddad Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: A PROSPECTIVE COHORT STUDY Bone and Joint Journal: 2018; 100-B:930–7.
- Shibanuma N, Ishida K, Matsumoto T, et al. Early postoperative clinical recovery of robotic arm-assisted vs. image-based navigated Total hip Arthroplasty. BMC Musculoskelet Disord. 2021;22(1):314.
- Piazza S. Designed to maintain collateral ligament stability throughout the range of motion. Stryker-Initiated Dynamic Computer Simulations of Passive ROM and Oxford Rig Test. 2003.
- Wang H, Simpson KJ, Ferrara MS, Chamnongkich S, Kinsey T, Mahoney OM. Biomechanical differences exhibited during sit-to-stand between total knee arthroplasty designs of varying radii. J Arthroplasty. 2006;21(8):1193-1199. doi:10.1016/j.arth.2006.02.172
- Gómez-Barrena E, Fernandez-García C, Fernandez-Bravo A, Cutillas-Ruiz R, Bermejo-Fernandez G. Functional performance with a single-radius femoral design total knee arthroplasty. Clin Orthop Relat Res. 2010;468(5):1214-1220. doi:10.1007/s11999-009-1190-2
JR-MKOSYM-OTHW-747688
Copyright © 2023 Stryker